- Joined
- Oct 9, 2010
- Messages
- 191
- Reaction score
- 109
NF CASE #12
Postoperative Fast HR
Night float quote of the week from one of my former senior residents:
"It's the same thing everywhere - you're there all by yourself, people crashin' and crumping, no one's there to help you, and you just gotta make **** happen."
========================================================================================================================================
Links to previous cases:
Case 1 Case 2 Case 3
Case 4 Case 5 Case 6
Case 7 Case 8 Case 9
Case 10
Case 11
====================================================================
49-year-old male 3 days s/p bariatric surgery.
PA covering general surgery floor calls you at 2:00am:
"Yeah this guy's heart rate is outta control, like 140 to 160. The EKG says it is sinus though. He's having some chest pain though. I gave him some nitro and it didn't help. Labs are normal. Can you come look at him?"
You check his labs real quick (ordered 30 minutes ago and just resulted):
- Electrolytes including ionized magnesium and calcium: All normal and K+ is 4.0
- Hemoglobin: 10.2 (was 9.8 yesterday, 10.1 day before)
- POC troponin: Undetectable
- nT-pro-BNP: Normal
You go see him. He is diaphoretic and clutching his chest.
His BP Is 151/102; SpO2 is 100%.
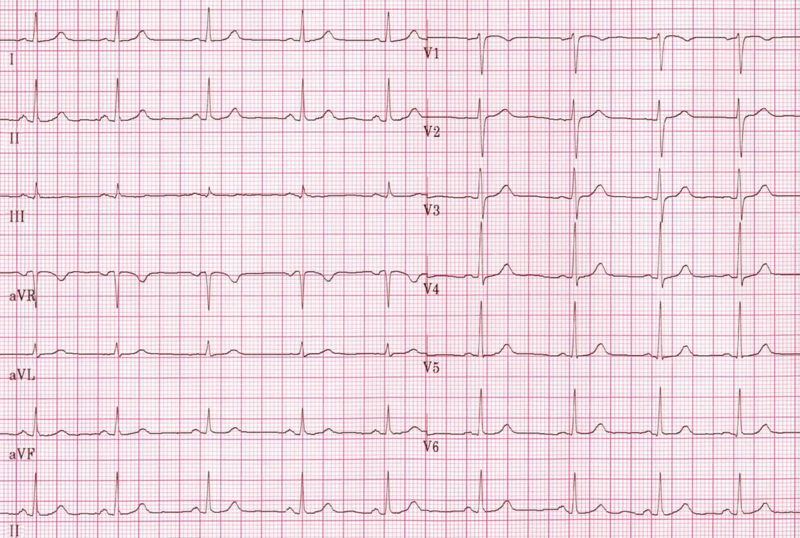
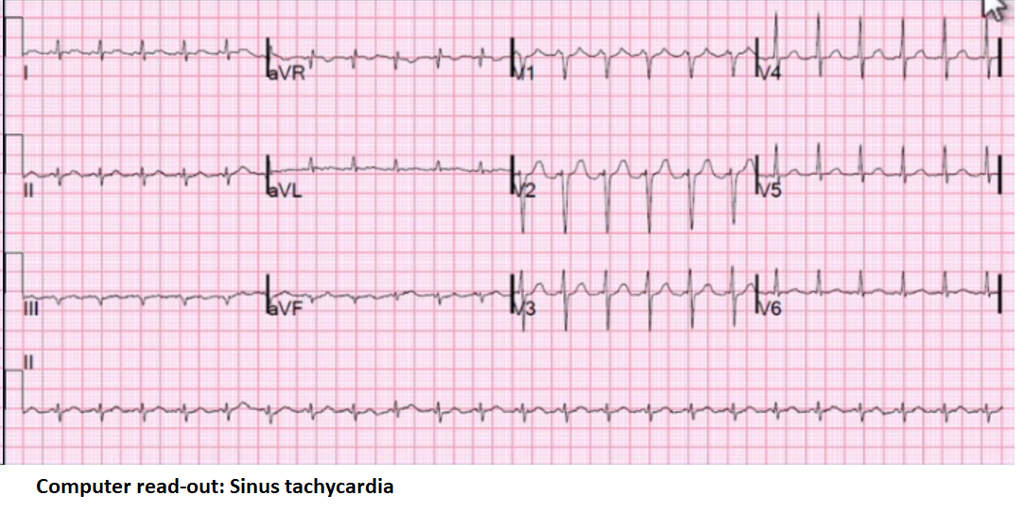
You glance at the EKG:
3 nurses and 2 techs are in the room freaking out, PA is nowhere to be found. What do?
========================================================================================================================================
UPDATE 1
UPDATE 2
UPDATE 3
RESOLUTION
Postoperative Fast HR
Night float quote of the week from one of my former senior residents:
"It's the same thing everywhere - you're there all by yourself, people crashin' and crumping, no one's there to help you, and you just gotta make **** happen."
========================================================================================================================================
Links to previous cases:
Case 1 Case 2 Case 3
Case 4 Case 5 Case 6
Case 7 Case 8 Case 9
Case 10
Case 11
====================================================================
49-year-old male 3 days s/p bariatric surgery.
PA covering general surgery floor calls you at 2:00am:
"Yeah this guy's heart rate is outta control, like 140 to 160. The EKG says it is sinus though. He's having some chest pain though. I gave him some nitro and it didn't help. Labs are normal. Can you come look at him?"
You check his labs real quick (ordered 30 minutes ago and just resulted):
- Electrolytes including ionized magnesium and calcium: All normal and K+ is 4.0
- Hemoglobin: 10.2 (was 9.8 yesterday, 10.1 day before)
- POC troponin: Undetectable
- nT-pro-BNP: Normal
You go see him. He is diaphoretic and clutching his chest.
His BP Is 151/102; SpO2 is 100%.
You glance at the EKG:
3 nurses and 2 techs are in the room freaking out, PA is nowhere to be found. What do?
========================================================================================================================================
UPDATE 1
UPDATE 2
UPDATE 3
RESOLUTION
Last edited: