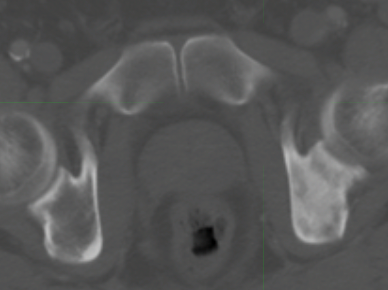
Guy in his 50s with newly diagnosed prostate cancer. GS 4+5 x 1, GS 4+4 x 3 cores, PSA 47, met to scapula and left ischium.
Wanting to treat prostate and bone mets with radiation. Would you treat the ischium and prostate separately or together? SBRT both? Hypofx both? Hypofx prostate and SBRT ischium?
Wanting to treat prostate and bone mets with radiation. Would you treat the ischium and prostate separately or together? SBRT both? Hypofx both? Hypofx prostate and SBRT ischium?
