- Joined
- Jun 16, 2021
- Messages
- 2,389
- Reaction score
- 2,627
Sent to me for a "stim trial."
COPD (1 PPD smoker), CAD/CHF, sleep apnea, cancer Hx, other Dx in his PMH.
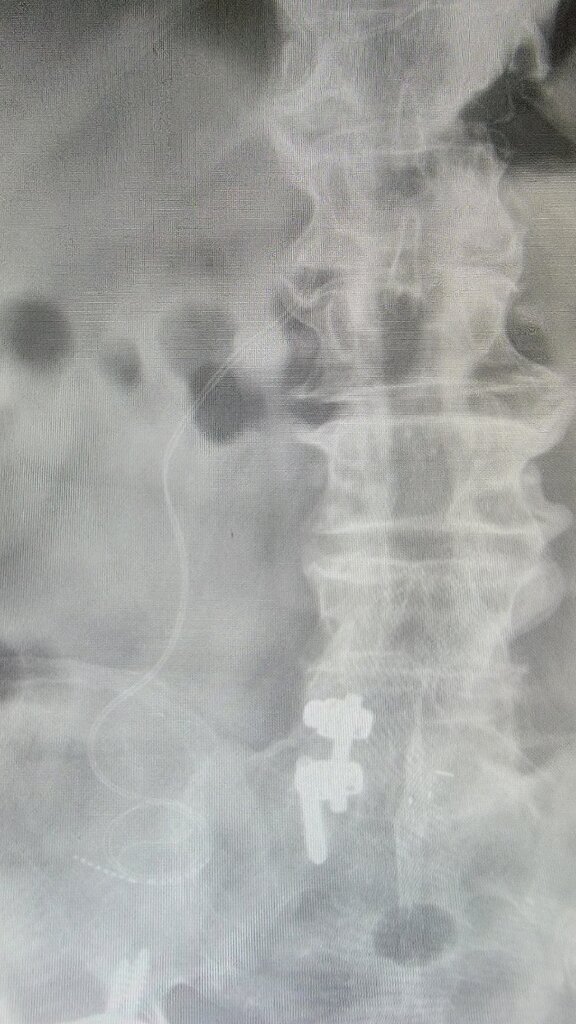
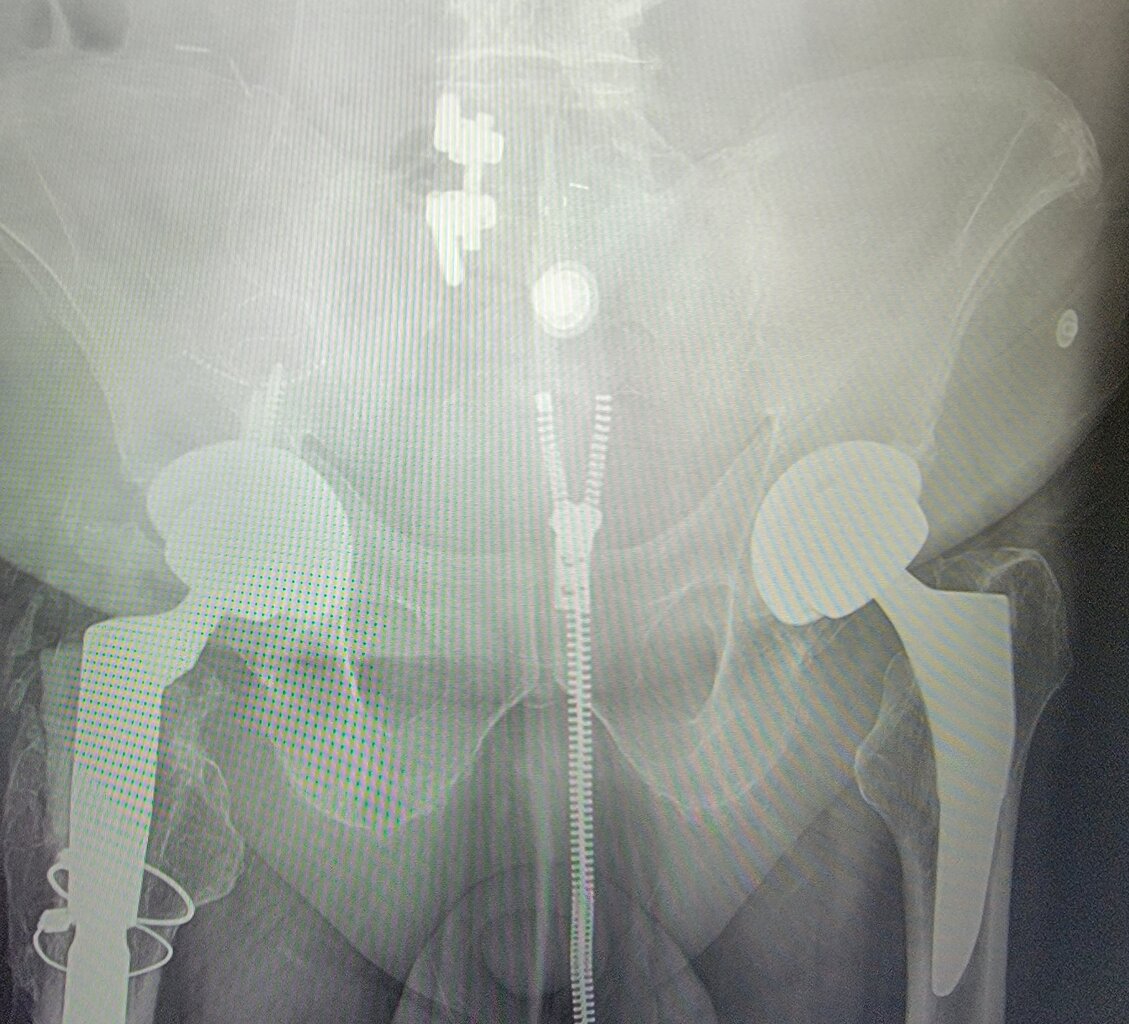
"I've had over 30 surgeries." Lumbar surgery x 5. Multi joint replacements.
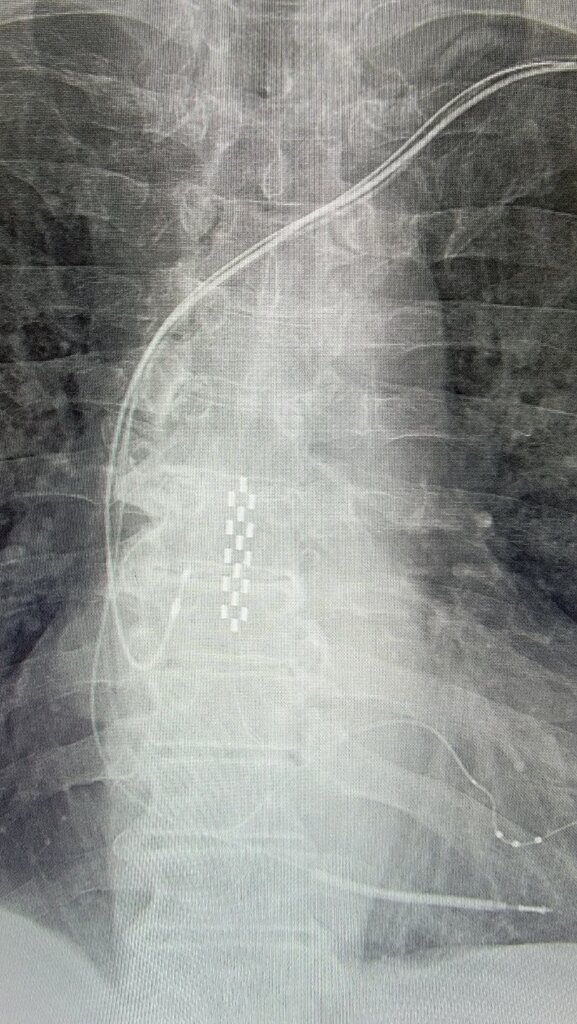
SCS implant with multiple revisions (at least 3). Initial implant op note reveals 3 levels of attempted paddle placement.
After all this BS - He has ITB/GTB pain.
COPD (1 PPD smoker), CAD/CHF, sleep apnea, cancer Hx, other Dx in his PMH.
"I've had over 30 surgeries." Lumbar surgery x 5. Multi joint replacements.
SCS implant with multiple revisions (at least 3). Initial implant op note reveals 3 levels of attempted paddle placement.
After all this BS - He has ITB/GTB pain.