- Joined
- Nov 21, 1998
- Messages
- 13,305
- Reaction score
- 7,969
- Points
- 8,231
- Location
- Over the rainbow
- Attending Physician
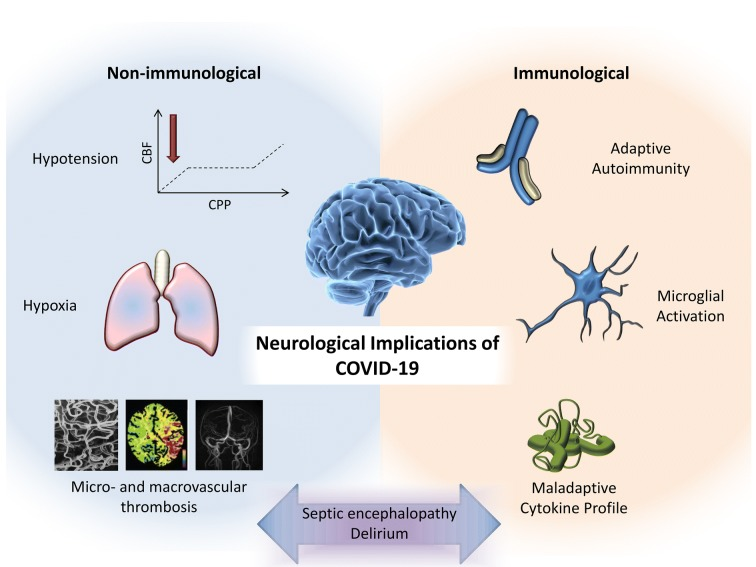
I think that I made my first diagnosis in clinic today on a woman diagnosed with COVID-19 in early March. PCR(+) and Ab(+) Moderate illness: Hospitalized 3 days and on supplemental O2 but no ventilator.
Developed sub-acute painful burning feet end of April. EMG shows mild sensorimotor peripheral polyneuropathy. No help from gabapentin, TCA's. Pregabalin caused edema. Tramadol causes twitching. Trialed low dose naltrexone and topicals. Trialed neutraceuticals and alpha-2-lipoic acid. Trialed acupuncture and TENS. Trialed Reikki, psilocybin, IV Ketamine, THC/CBD, and Shamanic Healing/Medical Intuitive Guided Healing/Spirit Animal.
Skin biopsy pending.
Question: DRG vs BurstDR vs HF10?
 neuropathycommons.org
neuropathycommons.org
Developed sub-acute painful burning feet end of April. EMG shows mild sensorimotor peripheral polyneuropathy. No help from gabapentin, TCA's. Pregabalin caused edema. Tramadol causes twitching. Trialed low dose naltrexone and topicals. Trialed neutraceuticals and alpha-2-lipoic acid. Trialed acupuncture and TENS. Trialed Reikki, psilocybin, IV Ketamine, THC/CBD, and Shamanic Healing/Medical Intuitive Guided Healing/Spirit Animal.
Skin biopsy pending.
Question: DRG vs BurstDR vs HF10?