- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
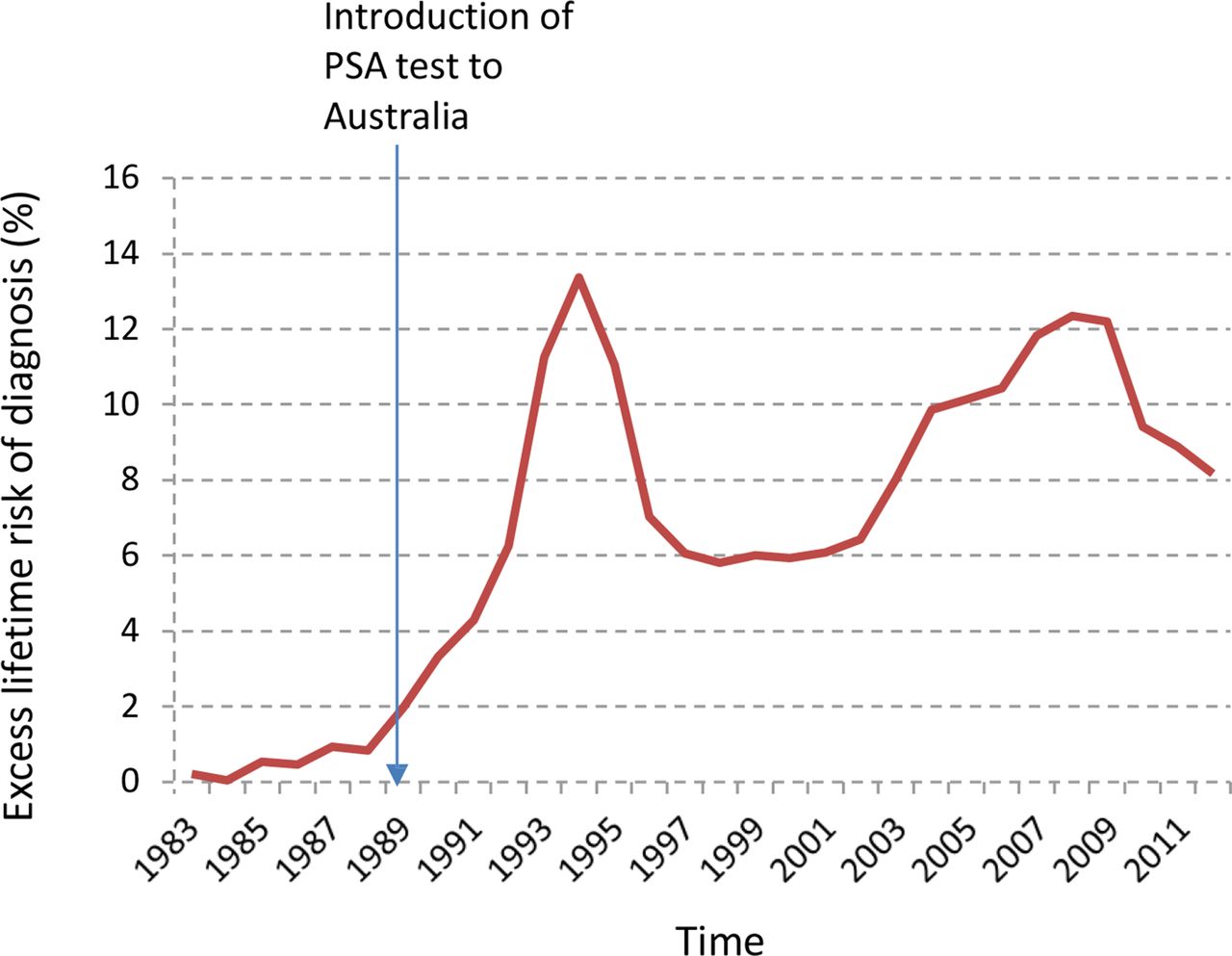
1) incidence of prostate cancer is significantly declining
2) “Many [proton center] business plans require treating men diagnosed with prostate cancer in order to make the proforma financially viable”
3) The NCDB covers about 70% of all newly diagnosed patients nationwide
4) From Emory U and NCDB data: 276,880 men received EBRT for T1-3N0 prostate cancer 2004-2015; ∴ 23,000/year
5) From Cornell and NCDB: 104,635 men with high risk T3/4 prostate cancer received EBRT 2004-2016 (and surgery incidence went from 23% to 41% in that timeframe); ∴ 8000/year
6) Assume ~50% overlap between #4 and #5, so add 50% of the yearly of #5 to #4: 23,000+4,000 = ∴ 27,000/year T1-4 prostates getting EBRT (or brachy or protons).... let's round to 30,000... and multiply by NCDB correction factor (1/0.7)...
Therefore 42,000 men, out of 191,000 newly diagnosed per year, getting radiation of some form for prostate cancer. I can recall when nearly a quarter million CaP were dx/year, when the population was smaller. (And again, this 42K/year is possibly a bit over-estimated.)
This is the second or third most common cancer, in theory, that should be being treated in radiation centers. And it works out to less than 8 prostate patients per rad onc per year? This is a utilization rate of 22% for prostate external beam. As stark as the numbers are they make sense because of previously quoted utilization rates falling and decreasing resident GU experience (24% decline last decade or so).
A number quoted as counter to 42K/year is 60K/year. If true, this would mean about 12 definitive prostate patients per year per rad onc instead of the eight I calc'd. Regardless, if a significant portion of radiation business relies on this very common cancer (which it does) which is becoming less commonly common and irradiated (which it is), the national profit margins for rad onc are getting thin and/or fragile. And APM will not help.
2) “Many [proton center] business plans require treating men diagnosed with prostate cancer in order to make the proforma financially viable”
3) The NCDB covers about 70% of all newly diagnosed patients nationwide
4) From Emory U and NCDB data: 276,880 men received EBRT for T1-3N0 prostate cancer 2004-2015; ∴ 23,000/year
5) From Cornell and NCDB: 104,635 men with high risk T3/4 prostate cancer received EBRT 2004-2016 (and surgery incidence went from 23% to 41% in that timeframe); ∴ 8000/year
6) Assume ~50% overlap between #4 and #5, so add 50% of the yearly of #5 to #4: 23,000+4,000 = ∴ 27,000/year T1-4 prostates getting EBRT (or brachy or protons).... let's round to 30,000... and multiply by NCDB correction factor (1/0.7)...
Therefore 42,000 men, out of 191,000 newly diagnosed per year, getting radiation of some form for prostate cancer. I can recall when nearly a quarter million CaP were dx/year, when the population was smaller. (And again, this 42K/year is possibly a bit over-estimated.)
This is the second or third most common cancer, in theory, that should be being treated in radiation centers. And it works out to less than 8 prostate patients per rad onc per year? This is a utilization rate of 22% for prostate external beam. As stark as the numbers are they make sense because of previously quoted utilization rates falling and decreasing resident GU experience (24% decline last decade or so).
A number quoted as counter to 42K/year is 60K/year. If true, this would mean about 12 definitive prostate patients per year per rad onc instead of the eight I calc'd. Regardless, if a significant portion of radiation business relies on this very common cancer (which it does) which is becoming less commonly common and irradiated (which it is), the national profit margins for rad onc are getting thin and/or fragile. And APM will not help.