You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Quadratus for Hips?
- Thread starter facted
- Start date
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
Is anyone doing QL for THR or arthroscopy? I've done it a bunch for anterior THR and it works really well but I'd like to get some input on traditional THR. Comparison to FIB? Thoughts?
Turns out the QL block gets the Lateral Femoral Cutaneous nerve without blocking the Femoral nerve allowing ambulation. A FICB typically involves motor weakness postop so is not desirable for some surgeons/patients wanting to ambulate the same day of surgery.
A QL block is better than FICB IMHO for preserving motor strength postop.
Facet I have done them but not consistently :/ Are you doing a bunch of these blade? I find that I vary my injection site somewhat based on anatomy/body-weight. It's more variable then a traditional tap. I would consider it for THA but I gotta calculate total dosing because our surg use exparel for joints. FI you would have to give even more local plus you have the motor component. Theoretically you can do QL for most procedures you would do a TAP block for.
- Joined
- Feb 8, 2007
- Messages
- 1,739
- Reaction score
- 291
- Points
- 5,356
- Attending Physician
I've done it a lot. Good results, almost immediately.
Did some today. Worked phenomenally well for thr. Used 25 of 0.5 bupi with 10ml saline and added 2mg dexamethasone. Neither pt received any narcs postop and have only gotten celebrex as part of post multimodal. Looks like a winner so far.
Did a ql1 on both.
Did a ql1 on both.
- Joined
- Jul 12, 2006
- Messages
- 4,755
- Reaction score
- 2,416
- Points
- 6,371
- Attending Physician
Good to know will try this 👍
- Joined
- Sep 4, 2004
- Messages
- 1,638
- Reaction score
- 1,748
- Points
- 5,056
Is anyone doing QL for THR or arthroscopy? I've done it a bunch for anterior THR and it works really well but I'd like to get some input on traditional THR. Comparison to FIB? Thoughts?
Hips don't really hurt that much anyways, but seems like an interesting idea...
We got rid of duramorph... No Foley's and worried about retention plus no need for pulse ox bed. Anterior hips are less painful for sure.Yes that is the "problem" For most of us doing spinal for total hips (plus duramorph) Is it worth it to do QL as well? Also how are you guys billing it?
- Joined
- Jul 12, 2006
- Messages
- 4,755
- Reaction score
- 2,416
- Points
- 6,371
- Attending Physician
More painfull in young patient than in old osteoporotic ladies.Hips don't really hurt that much anyways, but seems like an interesting idea...
- Joined
- Feb 8, 2007
- Messages
- 1,739
- Reaction score
- 291
- Points
- 5,356
- Attending Physician
How much local are you using green? 20cc? And are you doing the QL1/2 or the deeper one?
25-30cc, 0.5% bupi with 5mcg/ml epi, QL1/2 exclusively. Patients tolerate well and we get good views consistently. Great block.
Sent from my iPhone using SDN mobile
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
25-30cc, 0.5% bupi with 5mcg/ml epi, QL1/2 exclusively. Patients tolerate well and we get good views consistently. Great block.
Sent from my iPhone using SDN mobile
My only comment is to add some dexamethasone to improve duration of postop analgesia. I like the QL1 and QL2 approaches as well.
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
Is anyone doing QL for THR or arthroscopy? I've done it a bunch for anterior THR and it works really well but I'd like to get some input on traditional THR. Comparison to FIB? Thoughts?
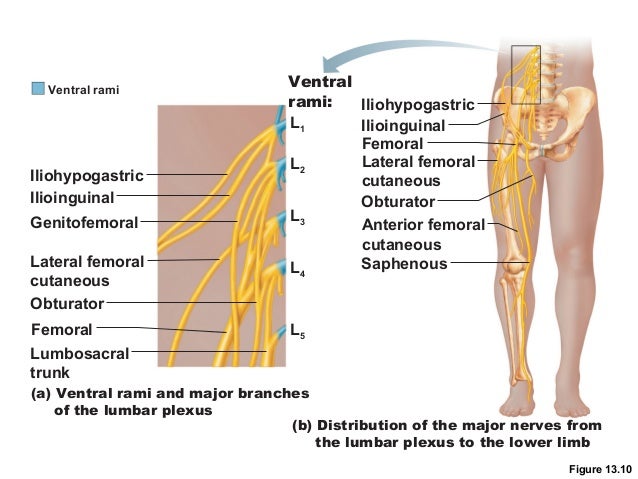
The genitofemoral and lateral femoral cutaneous nerves were dyed in a varying degree. No dye was seen to surround the lumbar plexus, femoral nerve or lumbar sympathetic trunk(figure 3)
THE PATHWAY OF INJECTATE SPREAD WITH THE TRANSMUSCULAR QUADRATUS... by Dr. Mette Dam
The Pathway of Injectate Spread With the Transmuscular Quadratus Lumborum Block: A Cadaver Study. - PubMed - NCBI (for those that get the A & A journal)
A radiologic and anatomic assessment of injectate spread following transmuscular quadratus lumborum block in cadavers. - PubMed - NCBI
A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. - PubMed - NCBI
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
25-30cc, 0.5% bupi with 5mcg/ml epi, QL1/2 exclusively. Patients tolerate well and we get good views consistently. Great block.
Sent from my iPhone using SDN mobile
Ultrasound-Guided Quadratus Lumborum Block: An Updated Review of Anatomy and Techniques. - PubMed - NCBI
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
All transmuscular quadratus lumborum blocks spread consistently to L1 and L3 nerve roots and within psoas major and quadratus lumborum muscles.
Look at the picture below as it regards the Lateral Femoral Cutaneous nerve. IMHO, that is the nerve we are likely "targeting" when we perform a QL block on a patient presenting for a total hip replacement (particularly the anterior approach).
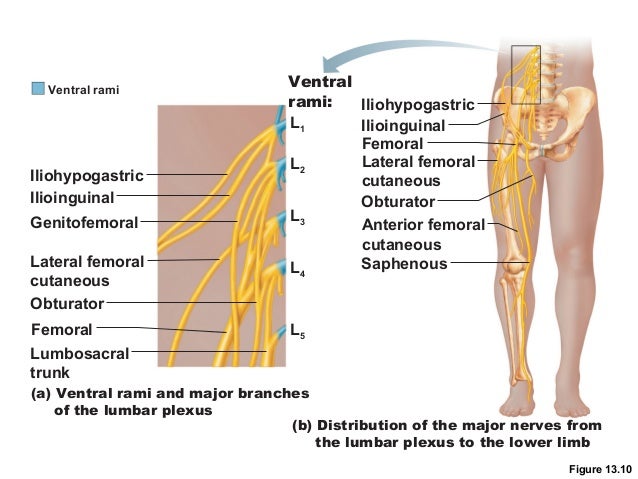
Look at the picture below as it regards the Lateral Femoral Cutaneous nerve. IMHO, that is the nerve we are likely "targeting" when we perform a QL block on a patient presenting for a total hip replacement (particularly the anterior approach).
- Joined
- Sep 4, 2004
- Messages
- 1,638
- Reaction score
- 1,748
- Points
- 5,056
More painfull in young patient than in old osteoporotic ladies.
Yes but you spinal them usually
Yea but for postop the block is still helpful. With duramorph I'm not sure, but without it looks like it makes a difference. Not sure where you guys are, but it surgeons are moving towards 23hr total joints eventually and duramorph is not ideal for that. A block that can provide 24 hr pain control with no motor block... Now that's more like it 🙂Yes but you spinal them usually
Yea but for postop the block is still helpful. With duramorph I'm not sure, but without it looks like it makes a difference. Not sure where you guys are, but it surgeons are moving towards 23hr total joints eventually and duramorph is not ideal for that. A block that can provide 24 hr pain control with no motor block... Now that's more like it 🙂Yes but you spinal them usually
- Joined
- Sep 4, 2004
- Messages
- 1,638
- Reaction score
- 1,748
- Points
- 5,056
Yea but for postop the block is still helpful. With duramorph I'm not sure, but without it looks like it makes a difference. Not sure where you guys are, but it surgeons are moving towards 23hr total joints eventually and duramorph is not ideal for that. A block that can provide 24 hr pain control with no motor block... Now that's more like it 🙂
But how do you know its providing pain relief vs the pain control is already sufficient with spinal and current techniques. THRs go well with a spinal and nothing else. For hips at least, pain is usually not limiting DC, without any block. So why bother? You could do straight GA for most hips and DC the person in 23 hrs.
- Joined
- Feb 8, 2007
- Messages
- 1,739
- Reaction score
- 291
- Points
- 5,356
- Attending Physician
Wouldn't say that, at least with our surgeons. Maybe surgical technique plays a role, but we spinal everyone and our pts without block still have pain even with multimodals.But how do you know its providing pain relief vs the pain control is already sufficient with spinal and current techniques. THRs go well with a spinal and nothing else. For hips at least, pain is usually not limiting DC, without any block. So why bother? You could do straight GA for most hips and DC the person in 23 hrs.
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
But how do you know its providing pain relief vs the pain control is already sufficient with spinal and current techniques. THRs go well with a spinal and nothing else. For hips at least, pain is usually not limiting DC, without any block. So why bother? You could do straight GA for most hips and DC the person in 23 hrs.
I agree with you. Most patients do fine without a block for an anterior hip replacement. Our surgeons inject local and the pain scores are good. Toradol/Dyloject plus Tylenol IV. I like dexamethasone 0.1 mg/kg IV as well.
That said, there are certain "high anxiety" types and those with pre-existing chronic pain or depression who would benefit from a QL block.
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
Blade if surg using 1 vial of exparel we would still be fine with an additional 25cc of .25% bup right.
No Problem. The Pacira rep is telling all the surgeons that the "max" is Exparel 266 mg plus one bottle of 0.5% Bupivacaine 30 mls. I think that's aggressive but I have gone along with it for patients over 70kg.
- Joined
- Oct 14, 2015
- Messages
- 171
- Reaction score
- 131
- Points
- 4,761
- Attending Physician
Is the CPT same as TAP block 64450?
This might be a worthwhile block for our group to add for patients who cannot receive a spinal or for the few surgeons who take 4 hrs to do a hip.
This might be a worthwhile block for our group to add for patients who cannot receive a spinal or for the few surgeons who take 4 hrs to do a hip.
- Joined
- Feb 8, 2007
- Messages
- 1,739
- Reaction score
- 291
- Points
- 5,356
- Attending Physician
Is the CPT same as TAP block 64450?
This might be a worthwhile block for our group to add for patients who cannot receive a spinal or for the few surgeons who take 4 hrs to do a hip.
I think that's how we are billing it.
Sent from my iPhone using SDN mobile
Is the CPT same as TAP block 64450?
Not a billing expert by any stretch but I believe it is coded as 64450 (other nerve block).
TAP is actually coded differently as of 2015:
New CPT Codes Take Effect
- Joined
- Oct 14, 2015
- Messages
- 171
- Reaction score
- 131
- Points
- 4,761
- Attending Physician
Not a billing expert by any stretch but I believe it is coded as 64450 (other nerve block).
TAP is actually coded differently as of 2015:
New CPT Codes Take Effect
Thanks for the FYI and link.
D
deleted162650
Look at the picture below as it regards the Lateral Femoral Cutaneous nerve. IMHO, that is the nerve we are likely "targeting" when we perform a QL block on a patient presenting for a total hip replacement (particularly the anterior approach).
If the goal is to hit the LFC, then a QL block seems like a roundabout way to get there. The LFC is easily visualized on U/S up high on the anterior thigh just below the ASIS. In fact, you've probably seen it every time you've done a Fem block, and just never knew it was there. In residency, we were actually trained to identify it when doing Fem caths (which we approached more laterally to give the cath more meat to travel through to avoid dislodgment) so as not to pierce it and leave the patient with a meralgia parasthetica. The LFC lives within the meat of the Tensor Fascia Lata which is the small spindle shaped muscle which lies right at the lateral border of the Sartorius. In the vast majority of patients, the nerve is seen as a hyperechoic point within the TFL. It'so easy to numb it here, which I have done for muscle biopsy cases.
- Joined
- Feb 10, 2013
- Messages
- 551
- Reaction score
- 392
- Points
- 5,276
- Attending Physician
Salty, I would appreciate a picture or a diagram. I've never seen the LFC on ultrasound.
Sent from my iPad using Tapatalk
Sent from my iPad using Tapatalk
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
If the goal is to hit the LFC, then a QL block seems like a roundabout way to get there. The LFC is easily visualized on U/S up high on the anterior thigh just below the ASIS. In fact, you've probably seen it every time you've done a Fem block, and just never knew it was there. In residency, we were actually trained to identify it when doing Fem caths (which we approached more laterally to give the cath more meat to travel through to avoid dislodgment) so as not to pierce it and leave the patient with a meralgia parasthetica. The LFC lives within the meat of the Tensor Fascia Lata which is the small spindle shaped muscle which lies right at the lateral border of the Sartorius. In the vast majority of patients, the nerve is seen as a hyperechoic point within the TFL. It'so easy to numb it here, which I have done for muscle biopsy cases.
Perhaps, the LFC nerve block is just as good as the QL block for postop analgesia after a hip replacement. At this point the QL block is just to new to know for certain. But, I'd be wary of doing any blocks in the vicinity of the surgeon's incision in case he/she injuries the nerve during the operation. I agree the LFC nerve is pretty far from the surgical incision of an anterior hip but they can get quite aggressive at times during the procedure.
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
Salty, I would appreciate a picture or a diagram. I've never seen the LFC on ultrasound.
Sent from my iPad using Tapatalk
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
- Joined
- Feb 10, 2013
- Messages
- 551
- Reaction score
- 392
- Points
- 5,276
- Attending Physician
Thanks blade!
- Joined
- Apr 16, 2005
- Messages
- 255
- Reaction score
- 44
- Points
- 4,581
bumping this thread from a year ago to ask some questions:
1. anyone ever place QL catheter? there are some case reports. Does the fact that it's a plane block make it ineffective due to needing too much volume? Maybe a programmed intermittent bolus pump would work better?
2. anyone done enough of these to know if they prefer "posterior TAP" lateral approach vs anterior injection between Psoas and QL vs posterior injection superficial to QL vs intramuscular injection?
3. anyone ever get motor weakness? I suspect case reports of motor weakness are due to accidental injection into the psoas muscle itself causing hip flexor weakness rather than weakness due to spread to motor nerves, but would like more experienced people with it to chime in
4. anyone do LFCN blocks after anterior total hip? I did a couple of these recently with success - much easier block as long as dressing isn't in the way
5. anyone able to get that consistent "unzip" image on u/s that looks so lovely to see with TAP blocks, with QL block? Sometimes I feel this is very challenging to achieve
1. anyone ever place QL catheter? there are some case reports. Does the fact that it's a plane block make it ineffective due to needing too much volume? Maybe a programmed intermittent bolus pump would work better?
2. anyone done enough of these to know if they prefer "posterior TAP" lateral approach vs anterior injection between Psoas and QL vs posterior injection superficial to QL vs intramuscular injection?
3. anyone ever get motor weakness? I suspect case reports of motor weakness are due to accidental injection into the psoas muscle itself causing hip flexor weakness rather than weakness due to spread to motor nerves, but would like more experienced people with it to chime in
4. anyone do LFCN blocks after anterior total hip? I did a couple of these recently with success - much easier block as long as dressing isn't in the way
5. anyone able to get that consistent "unzip" image on u/s that looks so lovely to see with TAP blocks, with QL block? Sometimes I feel this is very challenging to achieve
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
I think QL3 is the QL block most likely to get some motor weakness due to the vicinity of the Lumbar plexus. For that reason, I prefer QL1 or QL2 blocks.
Ortho Surgeons asked me not to do LFCN blocks on Anterior hips due to close proximity to incision. Hence, I do QL or Lumbar Plexus Blocks when needed for Anterior hips. Perhaps, the BEST solution is a T10 or L1 Erector Spinae Block? I can vouch that these ESP blocks work quite will with a catheter at 10 mls per hour.
https://www.jcafulltextonline.com/article/S0952-8180(17)31135-2/abstract
Ultrasound guided Erector Spinae Plane block at L-4 transverse process level provides effective postoperative analgesia for total hip arthroplasty
Ortho Surgeons asked me not to do LFCN blocks on Anterior hips due to close proximity to incision. Hence, I do QL or Lumbar Plexus Blocks when needed for Anterior hips. Perhaps, the BEST solution is a T10 or L1 Erector Spinae Block? I can vouch that these ESP blocks work quite will with a catheter at 10 mls per hour.
https://www.jcafulltextonline.com/article/S0952-8180(17)31135-2/abstract
Ultrasound guided Erector Spinae Plane block at L-4 transverse process level provides effective postoperative analgesia for total hip arthroplasty
Last edited:
- Joined
- Apr 16, 2005
- Messages
- 255
- Reaction score
- 44
- Points
- 4,581
I think QL3 is the QL block most likely to get some motor weakness due to the vicinity of the Lumbar plexus. For that reason, I prefer QL1 or QL2 blocks.
Ortho Surgeons asked me not to do LFCN blocks on Anterior hips due to close proximity to incision. Hence, I do QL or Lumbar Plexus Blocks when needed for Anterior hips. Perhaps, the BEST solution is a T10 or L1 Erector Spinae Block? I can vouch that these ESP blocks work quite will with a catheter at 10 mls per hour.
https://www.jcafulltextonline.com/article/S0952-8180(17)31135-2/abstract
Ultrasound guided Erector Spinae Plane block at L-4 transverse process level provides effective postoperative analgesia for total hip arthroplasty
I actually just did this (erector spinae) today for a postop hip with severe pain who wants to avoid opioids and whose surgeon does not want any motor weakness. I wanted to try T12 transverse process, but L4 was a lot easier to find and had what seemed like a clear plane between it and the overlying ES. I still found it challenging getting the ideal spread pattern, but eventually I think I got the bilateral lift. Pt reported significant pain improvement about 10 minutes after bolus of .125% bupi. No sensory dermatomal change in thigh. Put in a catheter and set at 8cc/hr. Had to pull it back to only 2cm beyond needle tip to get ideal spread pattern - hopefully doesn't dislodge
- Joined
- Apr 22, 2007
- Messages
- 22,923
- Reaction score
- 9,956
- Points
- 9,821
- Location
- Southeast
- Attending Physician
I actually just did this (erector spinae) today for a postop hip with severe pain who wants to avoid opioids and whose surgeon does not want any motor weakness. I wanted to try T12 transverse process, but L4 was a lot easier to find and had what seemed like a clear plane between it and the overlying ES. I still found it challenging getting the ideal spread pattern, but eventually I think I got the bilateral lift. Pt reported significant pain improvement about 10 minutes after bolus of .125% bupi. No sensory dermatomal change in thigh. Put in a catheter and set at 8cc/hr. Had to pull it back to only 2cm beyond needle tip to get ideal spread pattern - hopefully doesn't dislodge
Was this a classic/lateral/posterior Total Hip or the newer Anterior Approach? Post your follow-up for pain relief over the next 2 days (at my shop they go home POD1 or POD2).
- Joined
- Apr 16, 2005
- Messages
- 255
- Reaction score
- 44
- Points
- 4,581
it was young person who underwent a PAO (peri acetabular osteotomy) via scope
pt still has excellent pain control not requiring narcotics at all - just a little indomethicin to prevent heterotopic ossification and tylenol. Who knows if it might have been painless anyway - but family and pt are both quite happy
pt still has excellent pain control not requiring narcotics at all - just a little indomethicin to prevent heterotopic ossification and tylenol. Who knows if it might have been painless anyway - but family and pt are both quite happy
