If you had to bet:
In what cancer sites will radiation utilization go up in the next 10 years?
Bladder comes to mind. Maybe skin if Moh's gets severely clipped. That's all I got.
Utilization is going up in lung cancer; this is fact. This will be due to rising incidence of Stage I. This is good. However, compared to past, it will mean 5/6ths to 1/2 as many lung cancer patients under beam per day even though RT utilization is going up (SBRT less fx's than Stage III, natch). This is bad. And it seems there's a real "market cap" to SBRT in Stage I (which we are well away from hitting admittedly): lung cancer incidence is falling, and Stage I incidence can only go so high.
Skin has never seriously figured into RT utilization metrics; mostly because of the "1.8 million new cancer cases a year," non-melanoma skin cancer metrics are always outside this 1.8m (and not NCDB or SEER reportable usually). But yes, RT utilization could go up in skin.
Bladder seems more iffy to me, simply because urologists. But yes, it could. Renal? Maybe. Prostate, probably maxed out. Raw number of prostate patients has fluctuated wildly last decade, down and up. Thanks, USPSTF.
"RT utilization" (in the literature) has always only meant: if the patient is newly diagnosed with cancer, will RT be used within the first year of diagnosis? This has always seemed a pretty limited way to define RT utilization. Other things (ie how often will the patient come in for RT?) should have factored in for a more fulsome pic of RT utilization.
I think that's one reasonable interpretation. Conversely, one may also say "precision medicine" may eventually guide more patients to getting post-mastectomy radiation who need it, its not like its exclusively used for radiation omission (ie people are using decipher to push for more post op prostate).
Lets chew on this data. In the public NCDB database, use of radiation therapy in breast cancer is stable to increased from 2010 to 2019
The NCDB maintains benchmarking applications that have been developed to promote access to data by the general public, researchers, and clinicians.

www.facs.org
The number of fractions is going down, but I'm not so sure about the number of pts
View attachment 353290
View attachment 353291
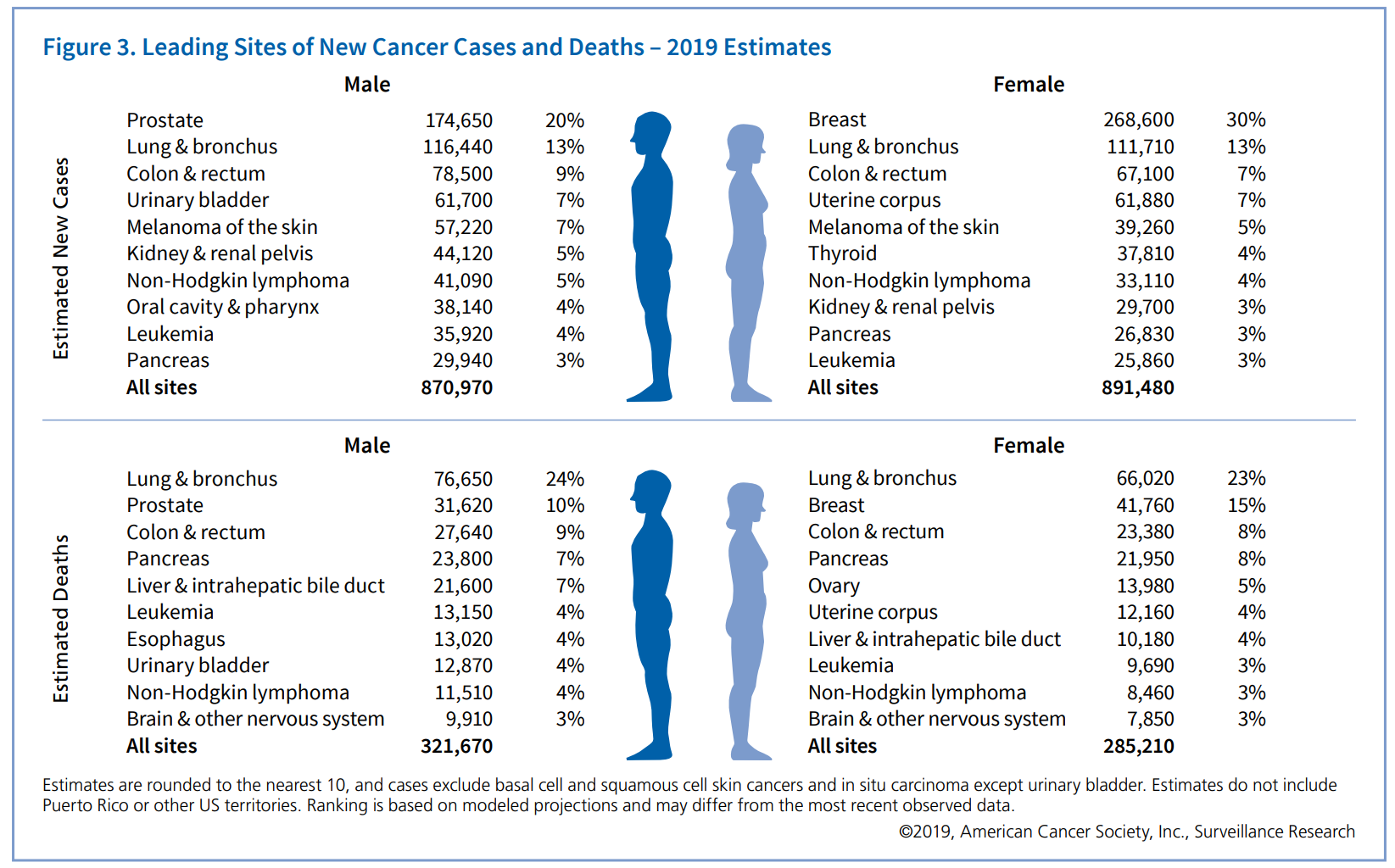
Great data. This shows:
1) RT utilization very stable over time (in breast)
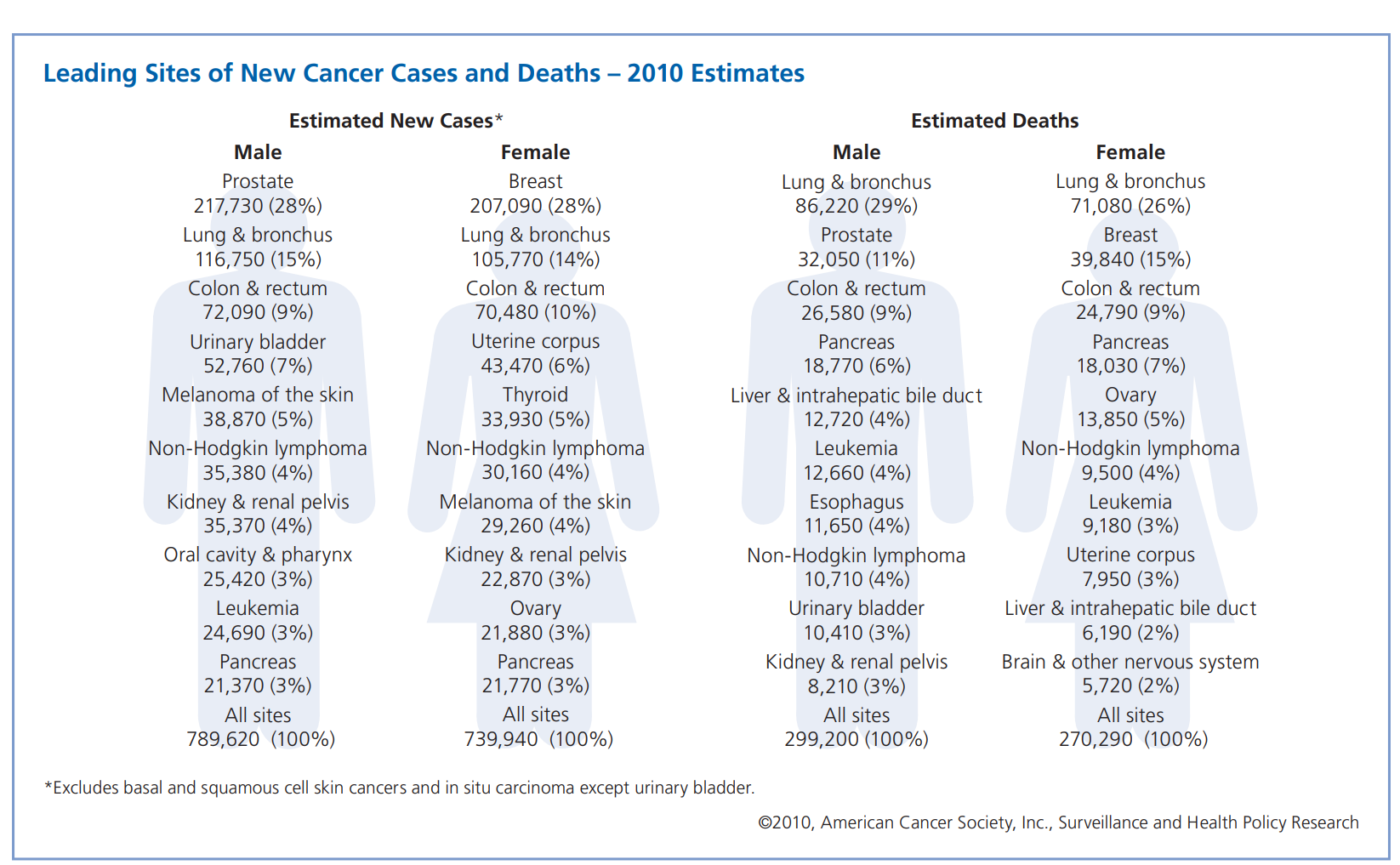
2) Raw number of breast RT patients up ~38% over 2010-19 (essentially: population growth, and more hospitals in 2019 vs 2010?). If we go nationwide ~207K cases in 2010, ~269K cases in 2019, we find a little more subdued growth of ~30%. But still, growth.
This looks good right? However, total rad oncs are up ~30-40+% (depending on where you look) over that time frame. And fractions are probably down a third, which means a third less patients under beam for breast ca per day in the US. Combined with hospital/center/rad onc "growth dilution," slightly less raw number of breast patients per rad onc (on average), less number of breast cancer patients "on the service" per rad onc on average.
Of course 1/3 (or more, now) of all rad oncs in America are employed by ~90 of the largest practices. They might have seen some growth or stability in "breast work" at the expense of the vast swath of low volume rad oncs/centers in the US, of which the majority of centers/rad oncs are.