- Joined
- Apr 3, 2019
- Messages
- 5,016
- Reaction score
- 11,505
- Points
- 5,601
- Attending Physician
The longer you stay the more you have to correct for time in the calcCome for the memes, stay for the alpha/beta calculations!
The longer you stay the more you have to correct for time in the calcCome for the memes, stay for the alpha/beta calculations!
I interpret this to be a matter of acceleration combating repopulation. For the most part, I BID all of my patients... but I am at a big academic center that treats for 12 hours a day on many machines, so it isn't a logistical hurdle for us (other than having two OTVs/week). From what patient's tell me, both 6-7 weeks QD vs. 3 weeks BID both kinda suck equally. If they are coming in from out-of-town, BID is actually better for them.Again on paper alpha beta wise what a huge jump in RBE from 45/30 to 66 or 70 qd. And they yielded bupkis. And then we do one dose escalation trial of bid and it’s positive. It’s almost like the SCLC data is trying to tell us BID works. If you have a plan where cord or lung or heart constraints can’t be met with 70 Gy RX dose, 45 Gy is such a friend.
Highlighted are radiotherapy theories from the 1980s, theories that haven't been invalidated yet.I interpret this to be a matter of acceleration combating repopulation.
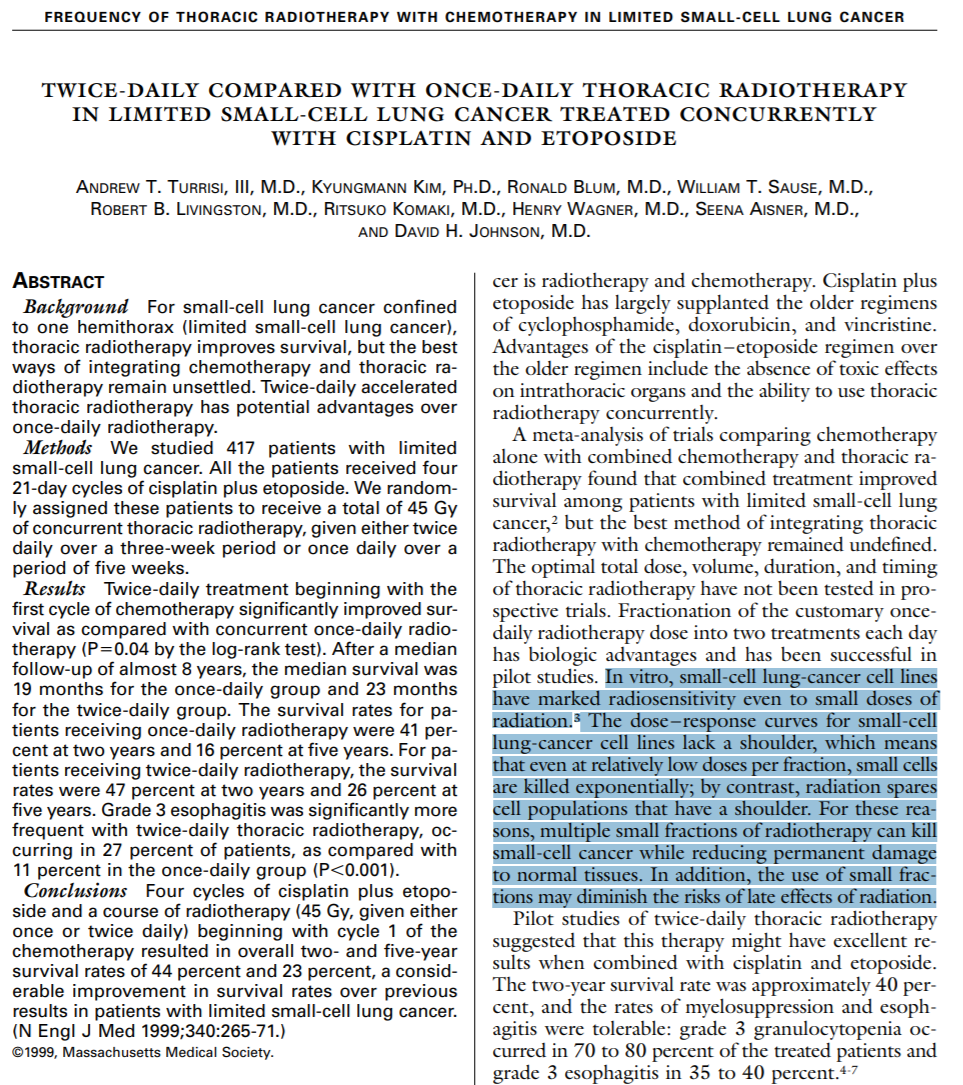
Great reference!Highlighted are radiotherapy theories from the 1980s, theories that haven't been invalidated yet.
Canadians do this and works fantastique!Will sometimes give 45/15 depending on volume
In other words, BID is the nickelback of bands. Sadly my patients never agree to it
We Asked Canadians Why They Hate Nickelback So Much And The Responses Are Hilariously SavageCanadians do this and works fantastique!
My go to es sclc consolidation doseWill sometimes give 45/15 depending on volume
Just a bunch of anonymous aholes complaining on the internet? I've heard that one before.
Been wondering if we could get away with 45 in 14.Will sometimes give 45/15 depending on volume
I heard GenSurg is running a non-inferiority trial reducing the number of sutures they use to close an incision. By using less Vicryl, they're not only reducing financial toxicity but also their carbon footprint. Do you really need more than two or three stiches to close an ex-lap? Seems wasteful.Been wondering if we could get away with 45 in 14.
In other news, on my way back from lunch I was wondering if gen surg has considered a trial of using constraints and a leather strap to bite down on in lieu of anesthesia. Slightly more acute toxicity but less financial toxicity I bet.
Prob should up the dose a bit to 70 if you're going to do QD but otherwise, there should be no problem compared to bid and we now have data to support that
I am sorry, but we had "data" before as well.
The CONVERT trial was negative. 66/2 QD was not superior to 45/1.5 BID and frankly, I think it looked a lot like inferiority for the QD-regimen.
Highlighted are radiotherapy theories from the 1980s, theories that haven't been invalidated yet.
Conceived by med onc turned rad onc Turrisi no less.for all the hate on radbio, it still amazes me to this day that this trial exists and was completed. Same dose once or twice a day is the most pure radbio experiment you could do and there was an OS difference. Imagine doing the equivalent med onc trial of a drug dose once or twice a day. I can think of no other pure radiation question in the field that has a phase III trial showing a survival benefit for a primary endpoint. Every other major trial has used chemo or hormones to get a survival benefit
If you're RTOG and Kian Ang (RIP), you take that data and make the failed regimen the standard arm for head and neck cancer for all future trials. See: RTOG 0129.Taking two trials testing superiority of a BED-escalated daily regimen, having that fail the primary end point, then saying "well it looks to be similar" is fair.
Taking it a step further and suggesting that once daily should be the preferred regimen or that it looks non-inferior is a statistical leap that I believe speaks to the biases of the posters in question more than it does in regards to the data.
I heard GenSurg is running a non-inferiority trial reducing the number of sutures they use to close an incision. By using less Vicryl, they're not only reducing financial toxicity but also their carbon footprint. Do you really need more than two or three stiches to close an ex-lap? Seems wasteful.
That reminds me - why aren't we trying to reduce our carbon footprint? Is penumbra really that important? Less flash/smaller field sizes means less electricity, which means we can save the polar bears. I'll start writing up the protocol, I'll name it something cute like POSTAGE-STAMP PORTAL 2112.
Good way of picking a treatment. Another way of reducing CO2 emissions would be picking a regimen with a worse OS.
Ah ha! Now we know that RO-APM was really an attempt to reduce America's carbon footprint.Good way of picking a treatment. Another way of reducing CO2 emissions would be picking a regimen with a worse OS.
I guess you want to go from probationary status to banned? Hey when you can't fight the facts, ad-hominem! Is that you, KO?
Here's another gem, completely divorced from the reality of clinical practice:
The same guy that hired an extender so he could get more Twitter time. I'm guessing he's salaried at Mayo, so hypofx is a win win for him for getting extra time with the bird.View attachment 345967
This is an absolute gem of a statement.
"[Hypofractionation] doesn't change the need for RadOnc, just the reimbursement." - Kenneth Olivier
In the context of "we're not training too many Radiation Oncologists". Man, I think one or two things have changed since March 12th, 2019. I don't want to pile on the other folks in that series of Tweets, so I'll just say that reading everything there is like opening a time capsule...and that wasn't even three years ago!
Taking two trials testing superiority of a BED-escalated daily regimen, having that fail the primary end point, then saying "well it looks to be similar" is fair. Offering it as an alternative to patients who can't/won't come for 45/30 BID is fair.
Taking it a step further and suggesting that once daily should be the preferred regimen or that it looks non-inferior is a statistical leap that I believe speaks to the biases of the posters in question more than it does in regards to the data.
There was once a phase II randomized trial improved OS. We (mostly) all treat oligomets now.
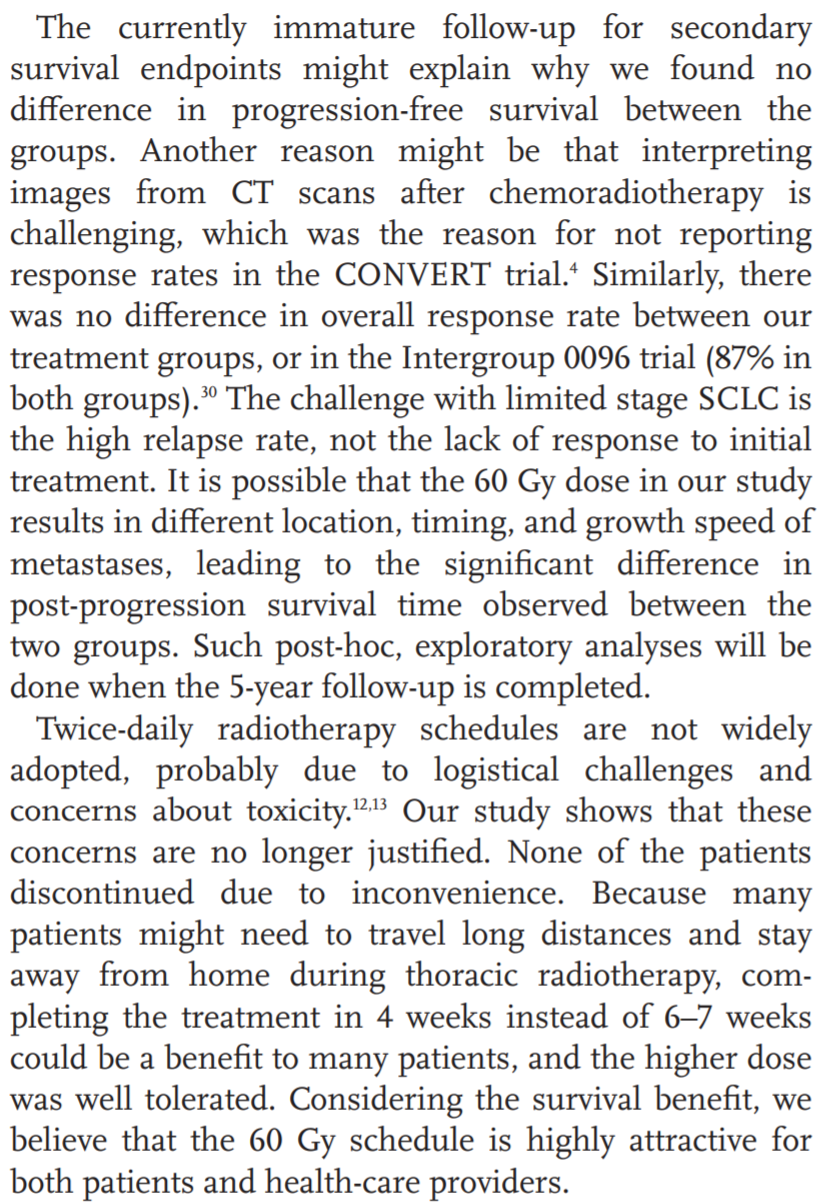
Now a phase II randomized trial also improved OS by tacking on 10 extra treatments. When it was presented last year, it didn't make sense because the PFS looked identical and OS was better - how did that happen, many (including myself) asked? But, there was an update in the paper. PFS improvement in 60/40 is numerically there, but P-value is like 0.13 or 0.067. They're underpowered for PFS. Somehow the median time from progression until death was longer in the 60Gy group. Unclear how that happened. But, they were (or at least seem to have been) powered for OS. P-value 0.012 on KM curves, with a goal of p < 0.1.
Better than P-value of 0.09 for OS in SABR-COMET KM curves, which was "statistically" significant because the goal was p < 0.20.
Canadians do this and works fantastique!
Maybe it’s that SCLC spreads the same regardless, but kills people slower with better thoracic control… or perhaps more RT improves non-cancer mortality 🤣How can you be underpowered for PFS, when it is a more commonly occurring event than seen with OS? That doesn’t make sense.
Am I incorrect in my understanding?
Maybe it’s that SCLC spreads the same regardless, but kills people slower with better thoracic control… or perhaps more RT improves non-cancer mortality 🤣
You guys are missing a killer marketing opportunity. Throw some solar panels on the roof and “go green while curing cancer”. “Killing cancer with the power of the Sun” and so on. You could even offer a package to offset their future CO2 use by planting one tree for every QALY gained.Good way of picking a treatment. Another way of reducing CO2 emissions would be picking a regimen with a worse OS.
So, the famous Urologist is picking on this radonc crowd.
Haha we are the "button pusher" and he recommends tri-modality for high-risk prostate ca.
I am so glad I don't know him IRL...
PS: The gen surgeons I trained with yrs ago did not consider Urologists surgeons lol...
So, the famous Urologist is picking on this radonc crowd.
Haha we are the "button pusher" and he recommends tri-modality for high-risk prostate ca.
I am so glad I don't know him IRL...
God wasted a perfectly good penis when he put ears on Matt Cooperberg*Cooperberg sure does seem like a winner. I hope he's not as ham-fisted in the OR as he is on Twitter.
45/15 is great. all things being considered I think that’s what makes the most sense, in many ways.
I *think* you are correct about power, assuming you are trying to detect the same HR for both PFS and OS. If I recall, a simple approximation of sample size is dependent on # events in the control arm… and PFS, by definition, will have the same or more events than OSWell that is a reasonable idea about how OS can improve without PFS or local control improving, which is what was seen in the trial, and to me doesn’t pass the smell test and deserves to be further explored to see if there is some mechanism here.
However my question was about the study being underpowered for PFS, which doesn’t make sense and is simply untrue based on my understanding of statistics.
well I will say this and say it sadly
45/15 makes a hellll of a lot more sense than 60/40 under the APM
Wasnt Walsh trial 2.67Gy x 15 directly to the entire esophagus with chemo?other than the concern for increased toxicity in terms of 3 Gy/fx to the esophagus with concurrent chemotherapy, radio biologically, I am not sure how 3 Gy/day, but giving it at one time, would be worse than splitting it up 6 hours apart at 1.5 Gy/fraction, in terms of tumor control
either way it is 45 Gy delivered in 3 weeks, which I think is probably the most important part of the treatment. would love to see this explored more.
I think people have started to lose the point of the original turrisi study which was that total dose in SCLC is less important than total number of fractions. Each time you give a fraction of treatment, whether it is 1.5 gy, 1.8 gy, 2 gy, 2.67 gy or 3 gy, you are likely getting some proportional cell kill that is roughly similar amongst the different doses because of a lack of shoulder. So going past 1.5 gy each fraction doesnt help you any more cell kill-wise, but extra dose beyond that goes to normal tissue. Thus, it makes the most sense to get the highest number of fractions in the shortest period of time for small cell given its doubling time. The total dose is likely less important.other than the concern for increased toxicity in terms of 3 Gy/fx to the esophagus with concurrent chemotherapy, radio biologically, I am not sure how 3 Gy/day, but giving it at one time, would be worse than splitting it up 6 hours apart at 1.5 Gy/fraction, in terms of tumor control
either way it is 45 Gy delivered in 3 weeks, which I think is probably the most important part of the treatment. would love to see this explored more.
You're going to bring an extensive stage patient in for 30-40 fractions? I'm notI think people have started to lose the point of the original turrisi study which was that total dose in SCLC is less important than total number of fractions. Each time you give a fraction of treatment, whether it is 1.5 gy, 1.8 gy, 2 gy, 2.67 gy or 3 gy, you are likely getting some proportional cell kill that is roughly similar amongst the different doses because of a lack of shoulder. So going past 1.5 gy each fraction doesnt help you any more cell kill-wise, but extra dose beyond that goes to normal tissue. Thus, it makes the most sense to get the highest number of fractions in the shortest period of time for small cell given its doubling time. The total dose is likely less important.
I am not sure why people would use 45 gy in 15 fx in any scenario (except for APM reasons). RTOG 0937 used 45/15 and that was a negative trial. The locoregional control was not particularly good plus it was toxic. Its just classic radonc to have a perfect radbio study showing fractionation actually matters and has a survival benefit, then just ignore it. Its also strange to me that BID regimens are not used in extensive stage and PCI (maybe hard to justify BID in mostly palliative cases)
Shout out to the OG Jeremic, who people probably thought 54 gy in 36 fx was crazy 30 years ago. But 17 month median OS for complete responders with some basic 2D radiation still ages pretty well (even in the atezo era)
View attachment 345990
I *think* you are correct about power, assuming you are trying to detect the same HR for both PFS and OS. If I recall, a simple approximation of sample size is dependent on # events in the control arm… and PFS, by definition, will have the same or more events than OS
other than the concern for increased toxicity in terms of 3 Gy/fx to the esophagus with concurrent chemotherapy, radio biologically, I am not sure how 3 Gy/day, but giving it at one time, would be worse than splitting it up 6 hours apart at 1.5 Gy/fraction, in terms of tumor control
either way it is 45 Gy delivered in 3 weeks, which I think is probably the most important part of the treatment. would love to see this explored more.
View attachment 345967
This is an absolute gem of a statement.
"[Hypofractionation] doesn't change the need for RadOnc, just the reimbursement." - Kenneth Olivier
In the context of "we're not training too many Radiation Oncologists". Man, I think one or two things have changed since March 12th, 2019. I don't want to pile on the other folks in that series of Tweets, so I'll just say that reading everything there is like opening a time capsule...and that wasn't even three years ago!
(Usually goes one of two ways)Maybe your pitch is better than mine, but they have no means to temporarily live closer to clinic, no interest in hanging out for 6 hours each day
This was the "take" I expected from the lung literati; and then I remembered, no one really "loves" the Turrisi study in the way that we seem to love other level 1 evidence. We are rad oncs, and here is a radiotherapy that offers increased survival (surpassing the unloved Turrisi study) for a very lethal cancer. You'd think we'd be rather enthused. Instead cold water was immediately dumped on the study's head by American rad oncs. We won't see another survival improving pure radiotherapy study of its sort maybe for another decade (or more). And to Ashwin Shinde's point, it should be f**king illegal that Evicore can say they won't approve it. It's one of the best examples we have where Evicore is killing people. (*NOT* hyperbolic.)Having had some time to think about it more, if a highly motivated healthier younger patient wanted to try it, I think there is enough there that I would be willing to discuss and perhaps include it as part of my standard initial consultation discussion.
Can also give radiation 4 hours apart as cord almost never a concern here.(Usually goes one of two ways)
Me: This is a cancer that's a little bit unusual in that we give radiation two times a day 6 hours apart.
Patient: OK.
Me: This is a cancer that's a little bit unusual in that we give radiation two times a day 6 hours apart.
Patient: I don't want to come in two times a day. Do I have to?
Me: No. We can treat once a day. But twice a day probably offers better survival and cure rates.
Patient: OK.
I once visited an RT clinic in Indonesia. A bus would bring rural patients in from surrounding villages in the morning like at 7 am. It wouldn't return until 5 to take them back home. Patients and their whole families would arrive, bringing snacks and sack lunches, prepared to encamp in and around the center for the whole day. They were seemingly happy, no one complained, etc.
This was the "take" I expected from the lung literati; and then I remembered, no one really "loves" the Turrisi study in the way that we seem to love other level 1 evidence. We are rad oncs, and here is a radiotherapy that offers increased survival (surpassing the unloved Turrisi study) for a very lethal cancer. You'd think we'd be rather enthused. Instead cold water was immediately dumped on the study's head by American rad oncs. We won't see another survival improving pure radiotherapy study of its sort maybe for another decade (or more). And to Ashwin Shinde's point, it should be f**king illegal that Evicore can say they won't approve it. It's one of the best examples we have where Evicore is killing people. (*NOT* hyperbolic.)
True. BTW for the residents, they came completely "off cord" in the Turrisi Intergroup study after 36 Gy (usually AP/PA to 36 Gy and the last 9 Gy using opposed tangents). Tx volumes were MUCH larger back then. They were very cautious about possible late side effects from hyperfractionating even though there was at least theoretical data at the time that small fraction sizes led to less late effects. The first mention of "linear quadratic" in the Red Journal was in the 1980s, the same decade this study started accruing. I can promise you that Andrew Turrisi could not do a BED calc at neither the start nor the finish of this study.Can also give radiation 4 hours apart as cord almost never a concern here.
A few comments. I think 45Gy / 30 is great. Constraints are easier to meet, looks to works as well or better than conventional fractionation. Patients deserve to be offered this if interested. I serve a very rural and poor population as part of my practice and they are categorically unwilling to travel for BID, so I am left to utilize alternatives for those patients. Maybe your pitch is better than mine, but they have no means to temporarily live closer to clinic, no interest in hanging out for 6 hours each day, and no local support organizations that can resolve these issues.
For those patients willing to do BID, I'm just not sure I'm willing to make the jump to 60Gy yet. I made a provocative statement earlier about "dragging" patients in for this, as I wanted to see what the defenders had to say. Would love for the effect to be real, and maybe it is. The PFS/OS thing is strange though and I just can't fully explain it away with what has been said so far.
When I pore over this study, I feel like there are a lot of small imbalances in the study that start to stack up.
In the 45Gy arm, there are more patients >70, worse ECOG, more current smokers, more with >5% weight loss.
View attachment 345992
I think this likely translated some to the treatment delivery side where you see less chemotherapy given, more dose reductions, more carbo given, and less people completing their radiation in the 45 Gy arm.
View attachment 345993
And then in the survival curves, you had a fairly immediate separation in survival, again I surmise due to some of these imbalances manifesting well before the treatment effect would be likely to manifest.
View attachment 345994
I think these imbalances undoubtedly magnified any benefit. Median survival in the 45Gy arm was 22.6 months, which compares unfavorably with CONVERT (30 months) and RTOG 0538 (29 months) (yeah yeah, cross trial comparison bad...). Also is a very small study at 170 pts and susceptible to a few outliers driving results. However, there does seem to be something going on here than can't be fully explained away either. Having had some time to think about it more, if a highly motivated healthier younger patient wanted to try it, I think there is enough there that I would be willing to discuss and perhaps include it as part of my standard initial consultation discussion. I can't say many of my small cell patients fit that bill, but always nice to have options as we attempt to maximize survival in a horrible disease. Ironically, these patients will be the most likely to have private insurance with higher probably of unpleasant evilcore interactions.
All this small cell talk probably needs another thread so we can keep appropriately gawking at radoncrocks twitter nonsense.
Probably about 4 things off the top of my head.'But twice a day probably offers better survival and cure rates.’
I don’t think we can accurately say this and be confident about it. What do you base this on?
Probably about 4 things off the top of my head.
First, the Intergroup. Better survival with 45/30 bid vs 45/25. Always this is met with cries of "inadequate control arm," but...
Second, every attempt at QD dose escalation, even up to 70 Gy, using larger fx sizes, has been bootless in toppling 45/30.
Third, why would we attempt going to beyond 60 Gy total doses in large-volume thoracic RT when we have data to suggest this decreases survival? That seems quite...weird...to be a fan of larger-fraction-size 66-70Gy for SCLC but eschew it in NSCLC.
Fourth, we now have the first dose-escalation data that did topple the OS of 45/30... and it's a twice a day regimen.
Again, to repeat, it seems like the data is attempting to show us that (small fx size) twice a day is good for SCLC.
I don't need to run a trial to show you that the OAR DVHs of a 45 Gy plan will be better than the OAR DVHs of a 70 Gy plan, do I?Yeah but both the 66 Gy and 70 gy trials, while
Not showing that it was BETTER, looked to beequivalentnot significantly different. I know, I know, not designed to be non inferiority trials.
But having two modern trials show thesame OSOSs not significantly different with daily vs BID is a far cry from showing that BID is BETTER!
