I'm your Huckleberry
From Bragg Peaks to Adaptive Fields—The Need for Evidence-Based Adoption of New Technologies in Radiotherapy
Nina N. Sanford, MD1;
Simul D. Parikh, MD2;
Matthew B. Spraker, MD, PhD3
Author Affiliations
Article Information
JAMA Oncol. Published online August 17, 2023. doi:10.1001/jamaoncol.2023.2931
In 2008, leading experts in proton radiotherapy argued that the superior dosimetric properties of protons compared with photon x-rays rendered randomized studies unethical,
1 an opinion that was espoused by commercial payers and community-based proton centers alike. Over the subsequent years, fueled by data from mostly single-arm clinical studies, dosimetric modeling, and financial interest, the use of protons expanded. As of 2023, there are 42 proton centers in the US.
Despite the purported benefit of the proton Bragg peak permitting sharp dose falloff, protons have been most widely used in disease sites that are common, such as breast and prostate cancer, but where the clinical impact of proton dosimetry is unclear.
2 Almost all of these patients have been treated off study, which contradicts recommendations from the American Society for Radiation Oncology (ASTRO) that proton radiotherapy to these sites should occur only in the context of a clinical trial or multi-institutional registry. Over time, reports emerged of unanticipated toxic effects from protons, such as radiation necrosis in pediatric patients with brain tumors,
3 severe radiation dermatitis and rib fractures in patients with breast cancer, and rectal injury in men receiving radiotherapy for prostate cancer.
4 These toxic effects, combined with rising costs, led to reconsideration of the need for comparative effective studies of proton radiotherapy. Randomized trials were finally designed for protons at the cooperative group level in sites such as the liver, esophagus, prostate, and breast. Unfortunately, because eligible patients were already being treated with protons off study, patient accrual has been challenging and may be skewed toward exclusion of patient subgroups who could potentially gain the most from proton radiotherapy. Without these studies, we will never know who proton radiotherapy benefits. This knowledge gap will disproportionately affect patients with socioeconomic risk. Although individuals with sufficient resources may continue to receive proton radiotherapy across disease sites, insurance denials due to lack of randomized data will preclude proton access for less privileged patients, even in scenarios where one may hypothesize there could be the greatest benefit to proton use.
More than 15 years later, we now find ourselves facing multiple opportunities to implement additional new technologies in radiation oncology, again with the premise of improving radiotherapy precision. Three relevant examples are adaptive radiotherapy platforms, magnetic resonance (MR)–guided linear accelerators, and devices that reduce the dose to adjacent organs. While some of these technologies have been prospectively tested, others have not, and we are concerned about the potential for uptake without proven superior effectiveness.
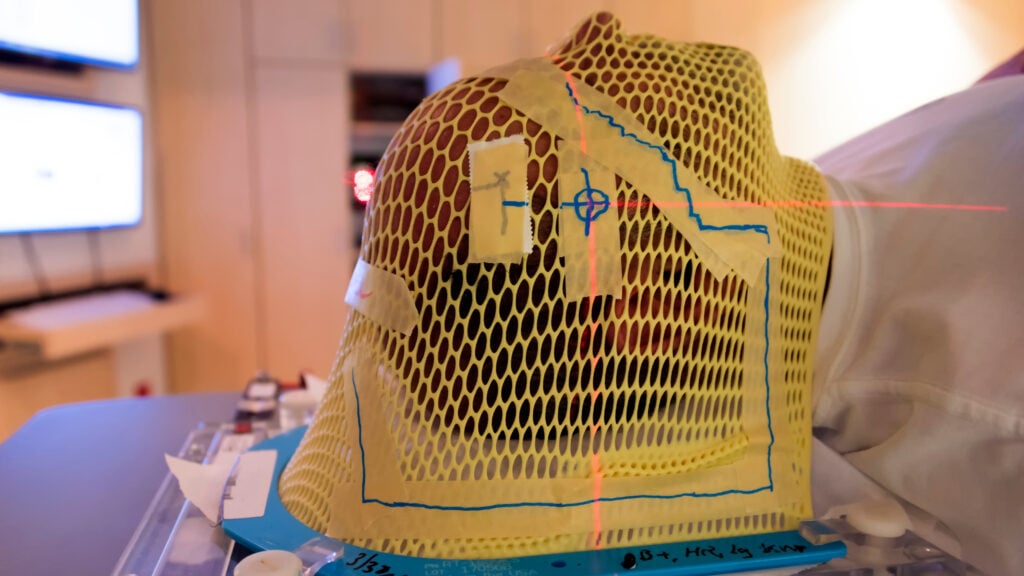
Adaptive radiotherapy (ART) refers to modifying the radiation volume or dose based on changes in tumor or organ position, size, or shape over the course of treatment. Compared with conventional radiotherapy, in which a static treatment plan is made at treatment outset, ART can optimize and modify plans periodically throughout the treatment course. In theory, if a radiotherapy plan can be adapted daily, higher doses could be delivered safely and outcomes may be improved. In practice, the on-table adaptive process can be time and labor intensive. With complex workflows, it is conceivable that a compounding of small changes or misses could cause deleterious outcomes. Currently, most studies supporting ART are retrospective and with dosimetric end points. A Prospective Study of Daily Adaptive Radiotherapy to Better Organ-at-Risk Doses in Head and Neck Cancer (DARTBOARD;
NCT04883281) is a phase 2 randomized trial of daily ART (with reduced treatment margins) vs nonadaptive radiotherapy in head and neck squamous cell carcinoma. The primary end point of the phase 2 study is xerostomia at 1 year. More randomized trials with meaningful, nondosimetric end points are needed.
Although most linear accelerators use computed tomography–based imaging guidance, recent advancements allow for MR-guided radiotherapy. The premise is that MR guidance offers superior soft tissue contrast, thereby improving visualization. In addition to the complexities described herein for ART, MR-guided radiotherapy comes with further challenges related to long treatment delivery time, patient claustrophobia, and motion management. As with ART, the demonstrated advantages of MR-guided radiotherapy are mostly in the form of retrospective or single-arm prospective studies. For example, in the single-arm Stereotactic MRI-Guided On-Table Radiation Therapy (SMART;
NCT03621644) trial of MR-guided adapted radiotherapy for locally advanced or borderline pancreatic cancer, the primary end point of treatment toxicity was benchmarked against historical controls. The promising outcomes of this study provide impetus for the upcoming randomized trial, Locally Advanced Pancreatic Cancer Treated With Ablative Stereotactic MRI-Guided Adaptive Radiation Therapy (LAP-ABLATE;
NCT05585554), which is powered to detect a survival benefit. Going forward, in disease sites with demonstrated safety and feasibility of MR-guided radiotherapy such as pancreatic cancer, studies should be randomized and have control arms receiving the current standard of care.
The third development is the hydrogel rectal spacer, which increases the physical distance between the prostate target and the rectum. Although randomized studies assessing this technology have been conducted, the authors of a recently published study
5 used an unvalidated dosimetry metric as their primary end point. In contrast, toxic effect databases from the manufacturer have revealed severe complications associated with spacer use that were not initially reported in the literature, and, as a result, some institutions in the US have halted their spacer programs.
Innovation is key in advancing the field of radiation oncology, and personalizing radiotherapy should be the goal of all radiation oncologists. There are many ways of personalizing therapy, ranging from the initial decision whether to treat with radiation to the timing of radiotherapy and integration with systemic therapy. Technologic advancements including ART, MR-guided therapy, and treatment devices represent one avenue of innovation, but thus far they have been adopted without sufficient compelling data. Radiation-IDEAL (R-IDEAL: idea, development, exploration, assessment, long-term study) provides a stepwise framework for evaluation of technologic innovations in radiotherapy.
6 Although modeling studies represent initial steps in development, the framework emphasizes randomization at an early stage and long-term toxic effect follow-up.
Yet there are several notable challenges in executing randomized trials of technologic advancements. First, they fall under a different regulatory framework than pharmaceuticals, which are required to meet an efficacy end point for approval. In contrast, technologies need only to show safety and “substantive equivalence.” At the same time, patients are bombarded with marketing initiatives. In a prior study,
7 a majority of patients demonstrated a fixed belief in the benefits of newer technology, with 74% indicating it was inherently superior to the established treatment. This phenomenon of technophilia may dissuade patients from agreeing to a randomized study that could assign them to an older technology they believe already to be inferior. Furthermore, some clinicians and hospitals with a vested interest in the new technology may believe that studies are not needed, and many are supported by funding from companies that could create conflicts of interest. In fact, since the capital has been spent, potential negative studies may cause economic harm to both the device manufacturers and the clinicians or hospitals that have invested in these technologies.
However, with already ample dosimetric data in support of ART, MR-guided therapy, and treatment devices, there is a critical need for multi-institutional prospective randomized trials assessing these technologies per R-IDEAL. For such trials to successfully accrue, radiation, surgical, and medical oncologists as well as patient advocates must champion enrollment, and studies should be supported by government or neutral parties. The uptake of proton radiotherapy without sufficient evidence has led to high out-of-pocket costs for patients, closures or imminent closures of many centers, and draconian prior authorization processes that hurt even those who stand to benefit the most from proton therapy. With rigorous prospective studies for these new technologies, we can avoid the mistakes made in the past and improve the therapeutic ratio of our radiotherapy treatments.