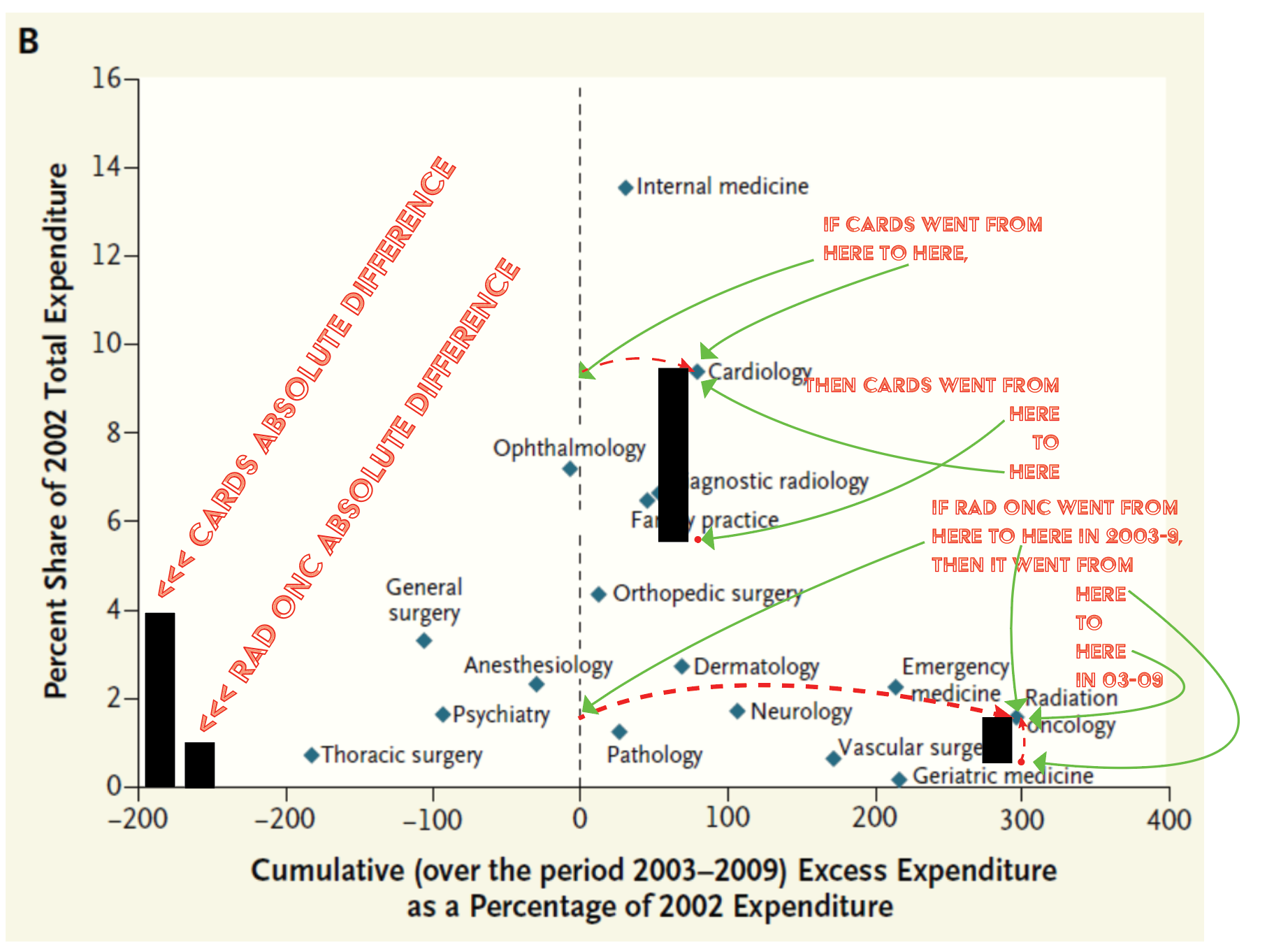
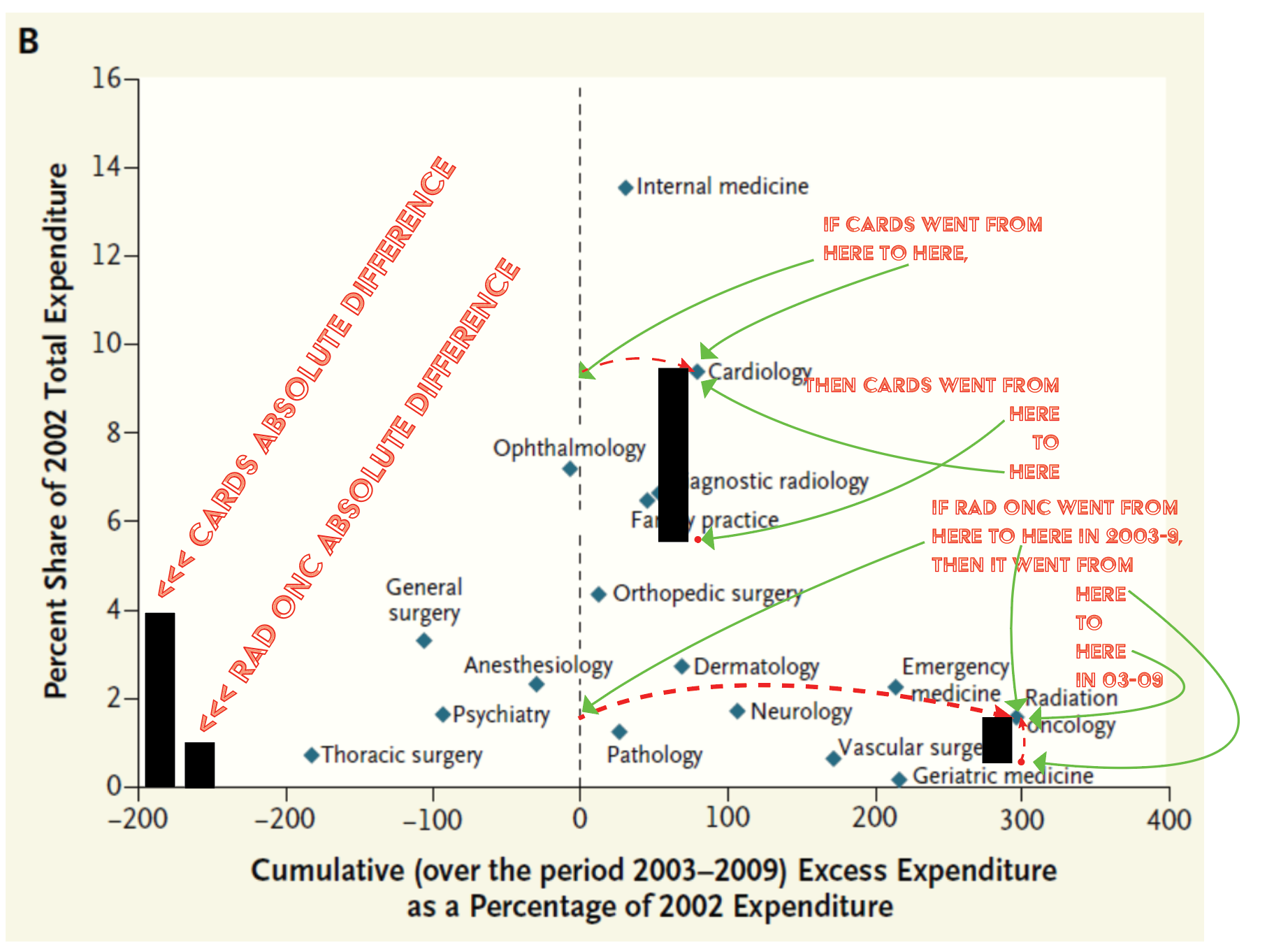
I have posted that here a few times... a good graph and a bad one...
Don't ever change. Looking forward to the manuscript!
I have posted that here a few times... a good graph and a bad one...
we need game theory in rad onc! Rad oncs vs tumors, rad oncs vs ABR, rad oncs vs racists, etc.
Astro spent all its effort trying to kill urorads. Then acandemic centers squeezed out and bought out private practices.
For its nobility, CMS rewarded rad onc with draconian cuts/bundles (and more to come!), academic centers could care two you know what’s about advocating for the speciality so lobbying dried up, and departments and chairs never looked up long enough to notice the “best and brightest” were basically being exploited for note labor and coverage.
If they decide to create hybrid diagnostic radiology / rad onc or IR/rad onc residencies then sure. Pure rad onc will be the same as nuclear medicine.Just in the past 5 years we have gone from derm level competitiveness to rads level to path level.....whats next? Nuclear medicine level?
Dermatology -> rads -> path ->Just in the past 5 years we have gone from derm level competitiveness to rads level to path level.....whats next? Nuclear medicine level?

In addition to “canaries in a coal mine”,Editor of red journal has been comparing radiation to syphilology for years. Do you know if it combined with ID?Dermatology -> rads -> path ->nuc medDermatology & Syphilology
EDIT extra haha bonus I see on right side of my screen w/ above link:

In addition to “canaries in a coal mine”,Editor of red journal has been comparing radiation to syphilology for years. Do you know if it combined with ID?
Don't think so. It just elegiacally suffused back into dermatology.In addition to “canaries in a coal mine”,Editor of red journal has been comparing radiation to syphilology for years. Do you know if it combined with ID?
Why, for the love of God, is no one in academia talking about creating a "clinical oncology" fellowship for radoncs? Neurologists can do a fellowship and give chemotherapy drugs, and we have far more oncology training than they do. They didn't do an entire internal medicine residency. GynOnc docs give chemotherapy. They didn't do an internal medicine residency or even an internship.
We've all see newly-minted heme/onc docs, and let's be honest: When they come out of fellowship, their solid-tumor knowledge and experience is not as strong as ours is.
My proposal: Radonc residency needs to go back to 3 years after internship. If Holman pathway residents can avoid at least a year of clinical training, then it's not really necessary, is it? Add an optional 2 year "clinical oncology" fellowship for those who want it so they can give chemo. Job issue solved.
Realistically it would be a very low number of people for the first decade or so. There would be enough time for a transition period. Many people would still end up doing 1 thing at the end of training (medonc or radonc, likely whatever is paying better at the time).I can't imagine how much worse it will be when you have heme/onc/med onc/rad onc potentially.
Job issue solved for the new grads. Job issue for us "old timers" begins anew. I agree with the proposal though.
I think the current batch of med oncs and rad oncs, would hate to compete with the dual certified physician. This may play a factor no? Essentially you are asking the people whose livelihoods would be threatened to create the very people who would take their jobs. For neuro-onc and gynonc I think they are "drumming up" more business for themselves so to speak. I admit, not sure who trains neuro-oncs (not much med onc involvement right?).
Lots of turf wars in med school between surg onc endo and ENT for thyroid related issues I recall with bad blood cross-training residents.
Again, not against the proposal and would love to have gotten the dual training myself, but if the current job market is already bad for rad onc, I can't imagine how much worse it will be when you have heme/onc/med onc/rad onc potentially.
Realistically it would be a very low number of people for the first decade or so. There would be enough time for a transition period. Many people would still end up doing 1 thing at the end of training (medonc or radonc, likely whatever is paying better at the time).
Indeed, that's the clinical oncologist in the UK.I think a dual trained rad/med onc would likely just be a rad onc who prescribed their own sensitizing therapy, rather than managing BMTs or some such thing.
I fully support such a pathway, the day after I retire.
Indeed, that's the clinical oncologist in the UK.
That's right. Speaking to my UK colleagues the clinical oncologists will prescribe the radio-sensitizing stuff, endocrine therapy and ADT whereas the medical oncologists will prescribe all the expensive novel agents.
In some countries the rad oncs will prescribe the concurrent chemotherapy even if they're titled as radiation oncologists.
There is no model in any country where a radiation prescribing doctor also prescribes all these novel agents. Not that I'm aware of anyways.
I am inclined to think radiation oncology in the US will be shotgun re-married to radiology.
A prior post brought up the excellent point that re-marriage would lead to the sudden demotion of many radonc department chairs. I can't see them enthusiastically embracing any model which leads them down that path.
Do most of them have a say in the matter?
All the ABR has to do is, after the ABR rad onc stakeholders agree, announce that there will be a hybrid DR/RO or IR/RO route and that for the next few years both conventional and hybrid pathways will exist but then only the hybrid pathways will remain. Just like how plastic surgery prevented general surgeons from doing a plastic surgery fellowship . Maybe they'll even call it an integrated therapeutic and diagnostic radiology residency program and make it six years.
And rad onc chairs at that time might be happy having junior attendings who can do both DR and RO.
They're chairs. They're safe. They're home and dry. They're over the hill. It's the junior / mid career one trick ponies that should worry.
A prior post brought up the excellent point that re-marriage would lead to the sudden demotion of many radonc department chairs. I can't see them enthusiastically embracing any model which leads them down that path.
History repeats itself... And comes full circle.A prior post brought up the excellent point that re-marriage would lead to the sudden demotion of many radonc department chairs. I can't see them enthusiastically embracing any model which leads them down that path.
There is one "hope". The introduction of novel agents that will alter radiation therapy effects - and only radiation therapy effects. When this takes place it may "upgrade" the role of radiation therapy in several indications and make it more competitive compared to surgery.That's right. Speaking to my UK colleagues the clinical oncologists will prescribe the radio-sensitizing stuff, endocrine therapy and ADT whereas the medical oncologists will prescribe all the expensive novel agents.
In some countries the rad oncs will prescribe the concurrent chemotherapy even if they're titled as radiation oncologists.
There is no model in any country where a radiation prescribing doctor also prescribes all these novel agents. Not that I'm aware of anyways.
I am inclined to think radiation oncology in the US will be shotgun re-married to radiology.

There may be a few of these agents, but let’s also not forget hpv cancers will be on their way out in the 2030sThere is one "hope". The introduction of novel agents that will alter radiation therapy effects - and only radiation therapy effects. When this takes place it may "upgrade" the role of radiation therapy in several indications and make it more competitive compared to surgery.
I am talking about things like:
- NBTXR3 in soft tissue sarcoma
- GC4419 in head and neck cancer
There are alot more compounds being tested nowadays, if these trials turn out positive we may be prescribing alot more drugs in the future.
Avasopasem manganese - Galera Therapeutics, Inc.
Avasopasem manganese (GC4419) is an investigational selective dismutase mimetic drug in development as a radioprotector in combination with radiation therapy (RT), with the goal to reduce side effects from radiation therapy. In preclinical studies, our selective dismutase mimetics significantly...www.galeratx.com
"Hello Mr. Schmidt. You have a locally advanced cancer of the tonsil. I am going to prescribe you 5 weeks of radiation therapy. Additionally you will receive compound X to mitigate any mucositis, compound Y to spare out any negative effects on your salivary glands and compound Z which will increase the effect of radiation therapy in the tumor without hurting any healthy tissue."
happy to be proven wrong but I don’t think there’s mature data that HPV vaccine prevents H&N cancer. Agree that it’s likely to do so.There may be a few of these agents, but let’s also not forget hpv cancers will be on their way out in the 2030s
Huh you may be right. I would have missed this question were it OLA ABR thoughhappy to be proven wrong but I don’t think there’s mature data that HPV vaccine prevents H&N cancer. Agree that it’s likely to do so.

Cervical cancer now easily falls under definition as a rare cancer.HPV driven cancers will have an incidence rate approaching 0 once the current generation realizes that having a libido is wrong.
Huh you may be right. I would have missed this question were it OLA ABR though

FDA Approves Gardasil 9 for Prevention of Oropharyngeal, Head & Neck Cancers Caused by HPV | CancerNetwork
The FDA approved an expanded indication for the HPV 9-valent vaccine, recombinant for the prevention of oropharyngeal and other head and neck cancers caused by HPV types 16, 18, 31, 33, 45, 52, and 58.www.cancernetwork.com
I haven't deep dived into the FDA announcement. Did they (ie Dr Hahn) give it that indication without direct data?The efficacy for cervical is quite impressive but I am unaware direct and not extrapolated data to support its efficacy in any other site. All big trials were cervix correct? Data I saw for other sites just subgroup analyses? Not saying I’m against giving it out, just not sure we shouldn’t run the studies like they did for cervical. Hopefully I’m wrong as vaccines for those sites would be great.
Not wrongHPV driven cancers will have an incidence rate approaching 0 once the current generation realizes that having a libido is wrong.

Anyone with libido will die of COVID before developing an HPV-related cancer!HPV driven cancers will have an incidence rate approaching 0 once the current generation realizes that having a libido is wrong.
You've harped on cervical cancer as rare before, but what definition of rare are you using? In the US, only 11 cancers may be "rare" depending on the definition.Cervical cancer now easily falls under definition as a rare cancer.
I don't know that there is a hard and fast rule. Cervical cancer's at about 13K cases/year now and trending to 10K/year soon. So we're talking about 2 cases per rad onc per year (on average)! It used to be more common, and there were less rad oncs. If e.g. there were 20K cases/year and only ~2500 rad oncs nationally (I think this would be the case circa 1990s), one can see more of a need to learn a lot about cervical ca and brachy. I "harp" on this because it is sad and depressing (and questionable?) that we spend so much time learning and training on cervical cancer but in reality most rad oncs are just never going to see it much, or at all. Sometimes 'round here we ask, "Why do we spend so much time learning peds?" Especially as it pertains to oral board exams etc. When looking at the incidences, and certainly the available cases per rad onc, we could soon start having the same discussions about non-pediatric cancers.You've harped on cervical cancer as rare before, but what definition of rare are you using? In the US, only 11 cancers may be "rare" depending on the definition.

Cervical cancer now easily falls under definition as a rare cancer.
If all the community rad oncs I interact with tell me that they treat "anything that walks in the door", well then every rad onc resident coming out needs to know how to treat "anything that walks in the door" unless we decide to change fundamentally as a specialty. In that case, you better get used to Ralph's way of thinking that every patient needs to be treated at a major center, because the only way to maintain that level of specialization is to have fewer rad onc centers with more docs who specialize in one or two disease sites.
You can't have it both ways. Even if cervical cancers and pediatric cancers are rare, you need to have the fundamentals down because you may end up treating them. Taking a curable (even if rare) cancer and having a patient fail treatment because you didn't know what to do is possibly the worst outcome of all for the patient. If you can't treat a cervical cancer walking out of residency, you'll be hopeless five years out.
This does assume that oral boards actually tests someone's competence. I've had the displeasure of working with two residents who told me to my face that they aren't interested in learning X, Y, and/or Z before going into general private practice, so just tell them what they need to know to pass boards. They did and they're in general private practice now. Some things you just can't fix, I guess.
Agree fully with this take. Especially in an unsure job market, you have no clue where you'll end up (it may not be a big city with the option of referring out) and what walks through that door.
Especially if you work in an area with high poverty. Some of these folks just don't have the support or means to get to the academic center.
This in my experience also encompasses pediatrics as well. I work in a "city" but the nearest academic center is at least a few hours away for some people. You can want to avoid treating peds as much as possible, but sometimes it's the only option for the patient.
This is highly dependent on where you practice.
Still don't think it needs to be on orals. If I don't know something these days I sure as hell know where to find it. The disproportionate amount of time required to master peds takes away from other higher yield sites.
Unless the external beam side is throwing off a lot of money it’s getting harder to justify economically keeping a brachy program up and running that hardly ever gets used. The falling cervical incidence and rising rad onc incidence means every rad onc has “access” to fewer and fewer patients. Treating anything that walks in the door is great. Unless it’s a huge financial drag to do so. A small drag is more handle-able, as was more widely achievable in a less oversupplied, higher CA incidence past. Again it’s all economics at work. Economics doesn’t care about our noble ideals. Being nakedly economic and only looking at number of cervical cases, number of rad oncs, and reimbursement, the average rad onc coming out today can expect to make what... $1500-2000/year (professional) doing cervical brachy? Maybe less? When you’re $400k in debt from med school it’s a big ask to learn all about cervical brachy’s that might walk through the door if that’s the volume/reimbursement you can expect. I know there are guys out there doing a lot of cervical brachy. That means there are way more that aren’t. And lots of new rad oncs and rad oncs to be that won’t.If all the community rad oncs I interact with tell me that they treat "anything that walks in the door", well then every rad onc resident coming out needs to know how to treat "anything that walks in the door" unless we decide to change fundamentally as a specialty. In that case, you better get used to Ralph's way of thinking that every patient needs to be treated at a major center, because the only way to maintain that level of specialization is to have fewer rad onc centers with more docs who specialize in one or two disease sites.
You can't have it both ways. Even if cervical cancers and pediatric cancers are rare, you need to have the fundamentals down because you may end up treating them. Taking a curable (even if rare) cancer and having a patient fail treatment because you didn't know what to do is possibly the worst outcome of all for the patient. If you can't treat a cervical cancer walking out of residency, you'll be hopeless five years out.
This does assume that oral boards actually tests someone's competence. I've had the displeasure of working with two residents who told me to my face that they aren't interested in learning X, Y, and/or Z before going into general private practice, so just tell them what they need to know to pass boards. They did and they're in general private practice now. Some things you just can't fix, I guess.
Unless the external beam side is throwing off a lot of money it’s getting harder to justify economically keeping a brachy program up and running that hardly ever gets used. The falling cervical incidence and rising rad onc incidence means every rad onc has “access” to fewer and fewer patients. Treating anything that walks in the door is great. Unless it’s a huge financial drag to do so. A small drag is more handle-able, as was more widely achievable in a less oversupplied, higher CA incidence past. Again it’s all economics at work. Economics doesn’t care about our noble ideals. Being nakedly economic and only looking at number of cervical cases, number of rad oncs, and reimbursement, the average rad onc coming out today can expect to make what... $1500-2000/year (professional) doing cervical brachy? Maybe less? When you’re $400k in debt from med school it’s a big ask to learn all about cervical brachy’s that might walk through the door if that’s the volume/reimbursement you can expect. I know there are guys out there doing a lot of cervical brachy. That means there are way more that aren’t. And lots of new rad oncs and rad oncs to be that won’t.
Thirty to forty years ago you could feasibly come out and establish a private practice (had to be right part of country, and you had to be a “go getter,” but still...) that was pure brachy. How awesome. How great. How sad that Ralph may be right (about brachy).I do more HDR for skin and breast ca (SAVI) than my partner does for gynecologic malignancies (she gets all of those). She does do a fair amount of interstitial brachy, though, as she does see advanced cases. She had an HDR prostate program set up for awhile, but with urorads in town she would only get a few cases a year.
Very tough to get the economics to work out for HDR brachy without expanding into skin and breast, I agree.
Agree, but probably more and more of it being done by a shrinking percentage population of ROs in practice, which is not a bad thing imo. High volume usually equals better outcomes all things being equal. Plus some places are just better equipped with good procedural suites, anesthesia support, in house MRI etcGyn brachy is not a dying skill... classic cervical Ca may be becoming rare, but think of all these endometrial recurrences, vaginal and vulvar cancers that need implant, inoperable endo
Gyn brachy is not a dying skill...
It is a dying skill. Per the ACGME, there is an "underutilization of brachytherapy for patients with cervical cancer and [an] associated decline in cure rates." It's like a dying language. In residency, we all learn the brachy Esperanto. But then we leave the confines of that bubble, go to different "countries," and then rarely get the chance to use the Esperanto again. It's not necessary for "conversation" like it was in the past. And with more rad oncs, the "incidence per rad onc" is even more of a downward slope than cervical ca incidence alone.*more of it being done by a shrinking percentage population of ROs in practice,

The studies also show that it's integral to curing cervical cancer and can't be replaced by ebrt. People should still be referring that outIt is a dying skill. Per the ACGME, there is an "underutilization of brachytherapy for patients with cervical cancer and [an] associated decline in cure rates."
Raising a big glass to @thecarbonionangle for this oneThe most imaginative guy in the bread line is still in the bread line.

Raising a big glass to @thecarbonionangle for this one

Are bread riots coming to America?
When people go hungry and the government refuses to help, sometimes they get madtheweek.com
