- Joined
- Apr 21, 2011
- Messages
- 3,761
- Reaction score
- 9,627
I think hemeoncs trying to deliver radiation therapy would lead to a whole new level of appreciation for radiation oncologists.
The hemeoncs that employ rad oncs and get a good chunk of their global have a level of appreciation even above that.I think hemeoncs trying to deliver radiation therapy would lead to a whole new level of appreciation for radiation oncologists.
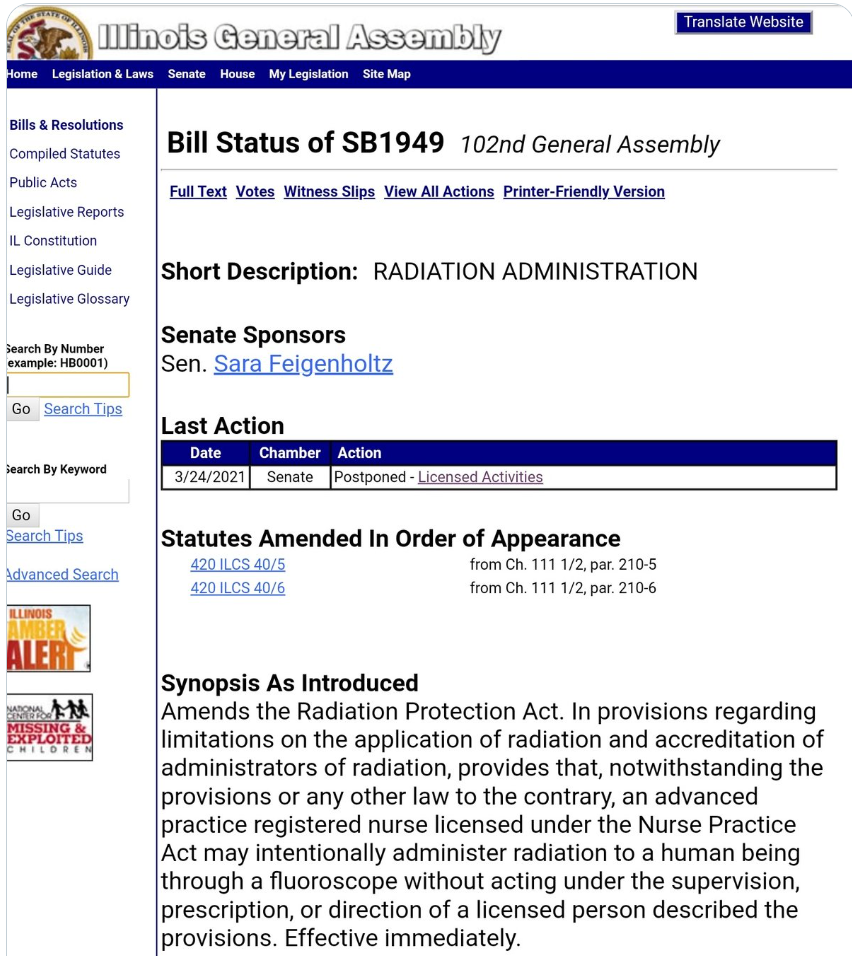
They mention in a later tweet they mistyped radonc as hemeonc here.Radiation Oncology's Plight,
In Three Acts
I. A senator sponsors a bill that has nothing to do with radiation oncology (except exceedingly tangentially)
II. A physician thinks the bill has to do with radiation therapy and that "HemeOncs" Rx radiation
III. Everyone starts fighting for the HemeOncs and their ability to prescribe RT
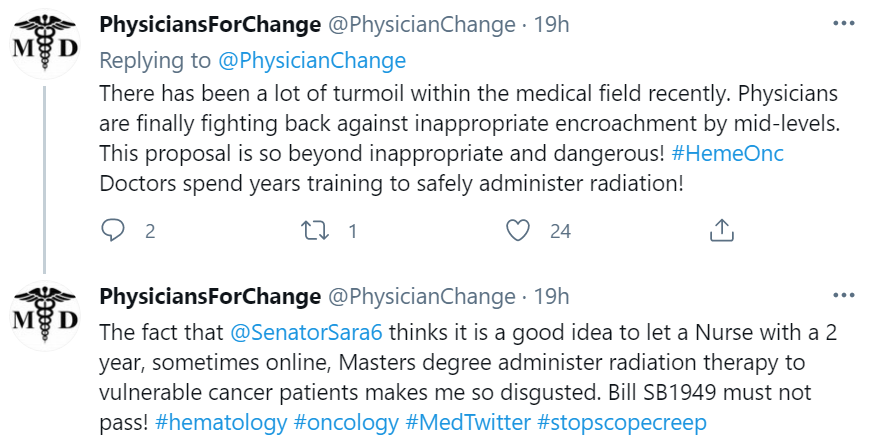
They “mistyped” it a few times lolThey mention in a later tweet they mistyped radonc as hemeonc here.
IIRC, Billy Loo at Stanford did it first. Basically an EP knocked on his door and ask if he thought RT could homogenize heterogeneous distributions of mixed scar/myocardium from prior MI. He tried it, it worked. A few other EP's got wind and started asking their rad oncs to try it.Question for the cardiac literati from the cardiac illiterati.
Before WashU did this for the first time, no one really had done it. So they theorized a way that would work, and I'll be darned it worked. But it was maybe one out of tens of different ways of doing this. So what are the chances that the WashU way is the only way? Did they just nail it on the first time by sheer force of latent cardiac know-how resting in the RO's brain or could it be that there might be actually numerous roads to Rome. Our man in the arena @OTN seems to have nailed it on his first try/tries too. My guess is that there's a panoply of approaches which will be minor variations on a theme that can (and will) be used to "blast" a big bolus of X-rays into the cardium and all of them work.
I foresaw that there would be “rad oncs” doing only heart in the future and got some guff. If this happens, to mis paraphrase Simul, “I left oncology; it didn’t leave me.”IIRC, Billy Loo at Stanford did it first. Basically an EP knocked on his door and ask if he thought RT could homogenize heterogeneous distributions of mixed scar/myocardium from prior MI. He tried it, it worked. A few other EP's got wind and started asking their rad oncs to try it.
Cliff and Phil were the first to protocolize it, and systematically test it.
There are a LOT of open questions, and Cliff & Phil are very open when they discuss the practice that there might be other ways to do it. Everything is cookie cutter right now to satisfy the cardiac division of the FDA, who is monitoring developments VERY closely, and has jurisdiction over trials, and device labeling indications.
I have treated a few of these patients with our team, and we opened a dose de-escalation trial at our institution, and I'm taking it with me to my next center (who is already treating a fairly decent volume), which will hopefully shed some insight onto whether 25Gy/1fx is really necessary, because that dose is obvious high risk to ultra-central tissues as well as gastric tissue (e.g. gastro-pericardial fistula that developed in one patient in the ENCORE-VT study), which is at risk if you don't gate.
@OTN is correct that from a rad onc perspective, the delivery is not nearly as challenging as the target delineation, which should never be done without an EP. The target delineation is made more challenging by the fact that EP's do not think about anatomy the way we do (slice by slice in one of the three cardinal axes). They think about anatomy from an endocardial structural point of view, so they are lost looking at anatomy the way we do, and vice versa.
The Wash U team puts on a phenomenal 2 day seminar/workshop every year, with hands-on practical sessions. If you're interested and have an interested EP, the best thing you can do is take them to this workshop.
There is probably just one RadOnc troll on Twitter, but gotta say, he is hitting where it hurts )
Because the solution to all problems in life is to throw money at it and hope the problem goes away. WTF Duke.
I've never seen URM outreach until the last year or so. Hell, Louis potters didn't exactly try to keep it a secret in his recent op-ed in the red journal.Ive seen a few of these URM med student rad onc scholarship opportunities now. Fundamentally, it is a good idea. It's an opportunity for students and departments to enter into a mutual beneficial arrangement. Student gets experience and exposure to the department and the department gets an opportunity to build a strong resident applicant and some research. However, the timing and optics of these could not be worse and that's the most damning evidence. Offering up a couple grand they poached off of junior faculty is transparent and unethical with the job market concerns.
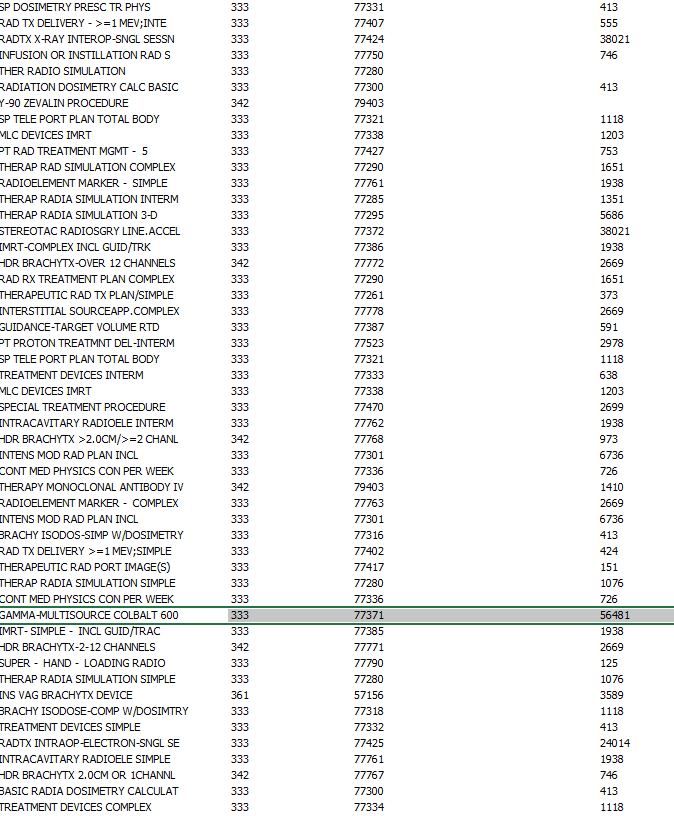
just wanted to post what emory has in terms of maximum prices:Railing on 30 Gy in 10 fractions for palliation, while meanwhile on the Emory proton therapy web page, they claim benefit for breast cancer, prostate cancer, rectal cancer, etc...
Page Not Found | Winship Cancer Institute of Emory University
We're sorry, this page has moved or has been deleted.winshipcancer.emory.edu
| Level 1 Therapeutic Radiation Treatment Preparation | 119 |
| Level 2 Therapeutic Radiation Treatment Preparation | 8055 |
| Level 3 Therapeutic Radiation Treatment Preparation | 22129 |
| Level 2 Radiation Therapy | 12759 |
| Level 3 Radiation Therapy | 27808 |
| Level 4 Radiation Therapy | 5313 |
| Level 6 Radiation Therapy | 41082 |
| Level 7 Radiation Therapy | 41082 |
Exactly. Truly altruistic action towards helping foster diversity in medicine includes mentoring/sponsoring students to succeed IN GENERAL while in medical school without regard for whichever specialty suits their individual goals.It’s not like increasing urm in radonc increases urm in medicine. They are just being diverted from fields where they are needed and would thrive and and shunted into a dead end speciality with no jobs.
Is it possible that everyone is being just a little too cynical here?Exactly. Truly altruistic action towards helping foster diversity in medicine includes mentoring/sponsoring students to succeed IN GENERAL while in medical school without regard for whichever specialty suits their individual goals.
US MD/DO applications to RadOnc are down =/= "time to increase diversity". The pool of available "diverse" applicants at the residency level remains constant; recruiting someone into RadOnc so they can struggle to find a job in a geographic area of their choice doesn't seem like you're recruiting them for THEIR benefit...
This whole thing feels so disingenuous to me. Where were these people currently beating the diversity drum 5 years ago when the average Step 1 score was >250? While the Twitter anonymous accounts can sometimes get a little aggressive, they do hit certain points with utter clarity: would you want to increase diversity on the Titanic?
Care to show us all the URM outreach and MS scholarships being offered by Stanford, Duke, UCLA etc 5-10 years ago?Is it possible that everyone is being just a little too cynical here?
Honestly, would be happy to when I am not quite so busy.Care to show us all the URM outreach and MS scholarships being offered by Stanford, Duke, UCLA etc 5-10 years ago?
I'm all ears
So max cost for a single sbrt fraction is $41K?just wanted to post what emory has in terms of maximum prices:
Tab Summary A B 1 Machine Readable Disclosure File 2 3 ...
Level 1 Therapeutic Radiation Treatment Preparation 119 Level 2 Therapeutic Radiation Treatment Preparation 8055 Level 3 Therapeutic Radiation Treatment Preparation 22129 Level 2 Radiation Therapy 12759 Level 3 Radiation Therapy 27808 Level 4 Radiation Therapy 5313 Level 6 Radiation Therapy 41082 Level 7 Radiation Therapy 41082
But if you're a program that's opening up a BS fellowship or expanding residency and recruiting URM, then F U.If programs were committing to cutting spots to a healthy amount and still offering URMs some opportunities like this it would be outstanding.
Why would anyone waste their time doing research to match the least competitive specialty?It is unfortunate timing as many people are still frustrated with the job outlook and over expansion, but if an URM is interested and still wants to pursue inspite of the issues then at least they’re getting paid to do some research.
There's no nefarious plot. Nefariousness usually implies a kind of Gru, Dr. No, Count Dooku underlying intelligence, and I do not give that much credit. It's laziness. It's a dog-ate-my-homework excuse. It's yet another example of radiation oncology('s leaders) failing and not dealing with the underlying problem. Diversity is a foil which is being used to cover the embarrassment/the fact that medical students aren't choosing radiation oncology anymore. What is bad, of course, is now this makes it even harder to reduce residency spots because a call to reduce residency spots may elide into somehow being an attack on trying to increase URMs in RO. Oh you want to reduce residency spots? You must be a real big Piers Morgan fan, huh? That will be a blow to the decrease residency spot movement if it happens that way.Honestly, would be happy to when I am not quite so busy.
I would also make the point that society has evolved in the past 1-2 years and diversity has become a greater priority in a lot of facets of medicine (i.e. departments now have 'Director of Diversity' positions). Perhaps this is more reflective of THAT trend rather than some nefarious plot lure URM into a world-class research lab.
To be clear, I absolutely do not think that anyone is doing anything nefarious. Honestly, I think virtually everyone, on every side of the argument, is really doing what they believe is "best" (though I'm sure there are a handful of bad actors, as with anything).Honestly, would be happy to when I am not quite so busy.
I would also make the point that society has evolved in the past 1-2 years and diversity has become a greater priority in a lot of facets of medicine (i.e. departments now have 'Director of Diversity' positions). Perhaps this is more reflective of THAT trend rather than some nefarious plot lure URM into a world-class research lab.
So max cost for a single sbrt fraction is $41K?
The legend goes that Emory charges more for SRS than any other center in the U.S. May be some truth to the legend?!they are trying to obscure the data
ZeaTool – A Healthcare Price Comparison Tool for ...
https://zeatool.com
ZeaTool is a CMS-compliant price transparency tool that has collected over 5,000 hospitals' CMS Price Transparency Data. If your hospital is not yet compliant
Tab Summary A B 1 Machine Readable Disclosure File 2 3 ...
https://www.emoryhealthcare.org › 110010-emory-...
XLS
Jan 1, 2021 — The first Is "gross charge" that relates to the established prices that are billed to all patients ... hospital charges for purposes of enhanced transparency and communication. ... 1, Hospital Name, Emory University Hospital.
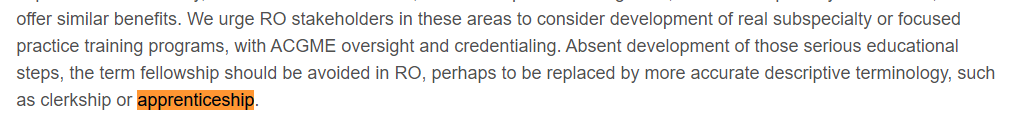
Name of the game is less high quality programs and no low quality programs.View attachment 335302
These guys are the chair and vice chair of the RRC. We will see. Going through other forums I get the impression that the acgme is actively hostile to high training standards for programs (just see ED) and are the root of the “we can’t do anything b/c of anti-trust” big lie.
Under Dr. Rosenzweig's leadership, Mount Sinai has grown from 6 total residents ten years ago to 12 currently (although only 10 are permanent positions per ACGME).Cutting spots, closing entire programs? I’m not holding my breath.
Upenn and Mount Sinai will continue to fill for a few years.
Upenn because it’s a good program and MS because it’s a 4yr job with benefits in NYC.
Those 2 docs have no real pressure for now
Under Dr. Rosenzweig's leadership, Mount Sinai has grown from 6 total residents ten years ago to 12 currently (although only 10 are permanent positions per ACGME).
Yep. Their perverse incentive is to train more radoncs. Ours is to treat more fractions. We should both choose wisely.Radonc resident training is just a business.
I think UPenn has also grown into 4-5 residents per year like Stanford, Emory and others.Under Dr. Rosenzweig's leadership, Mount Sinai has grown from 6 total residents ten years ago to 12 currently (although only 10 are permanent positions per ACGME).
Good news on the fractionation front: the government is on the case. For resident trainers, market will have to slowly teach authorities the right way.Yep. Their perverse incentive is to train more radoncs. Ours is to treat more fractions. We should both choose wisely.
If we're writing opinions based on analyses from 2011, wait till I tell you guys about these incredible calculations Ben Smith was working on called the "Rad Onc Undersupply", although in 2011, math seemed hard; and later all the calculations and analyses seemed necessary to have been erased from the face of the Earth in order to save some semblance of face.View attachment 335344
Me, internally: "What in the world is this"
*follows link*
View attachment 335345
"Ah, physics. Ok! Wait..."
View attachment 335346
If we're writing opinions based on papers from 2004, wait till I tell you guys about this incredible device Apple is working on called the "iPhone", although in 2004, the iPhone was still 3 years away from being announced.
'Tis comforting, to me anyways, physicists' grasp of math.There is currently a shortage of medical physicists in US
Follows supply and demand. About 10-15 years ago, board certification started requiring graduation from a certified medical physics masters/phd and a certified physics residency. Previosuly, In early 2000s, medical physics was open to any masters/phd physicist (from optics to solid state to nuclear) with 1-2 years of on the job training, who could then sit for board certification. Several years ago Dosimetry increased training requirements (certified masters) as well, which is why a dosimetrist in the bay area now earns more than a physician/instructor at Stanford.There is currently a shortage of medical physicists in US. Our network employs many, and is having trouble to recruit. No trouble hiring mid-career attendings
I personally will choose Dosimetry.What would be easier and/or have better job outlook - us retraining as radiologists or medical physicists?
The breadlines want to know
