- Joined
- Feb 10, 2016
- Messages
- 3,312
- Reaction score
- 6,150
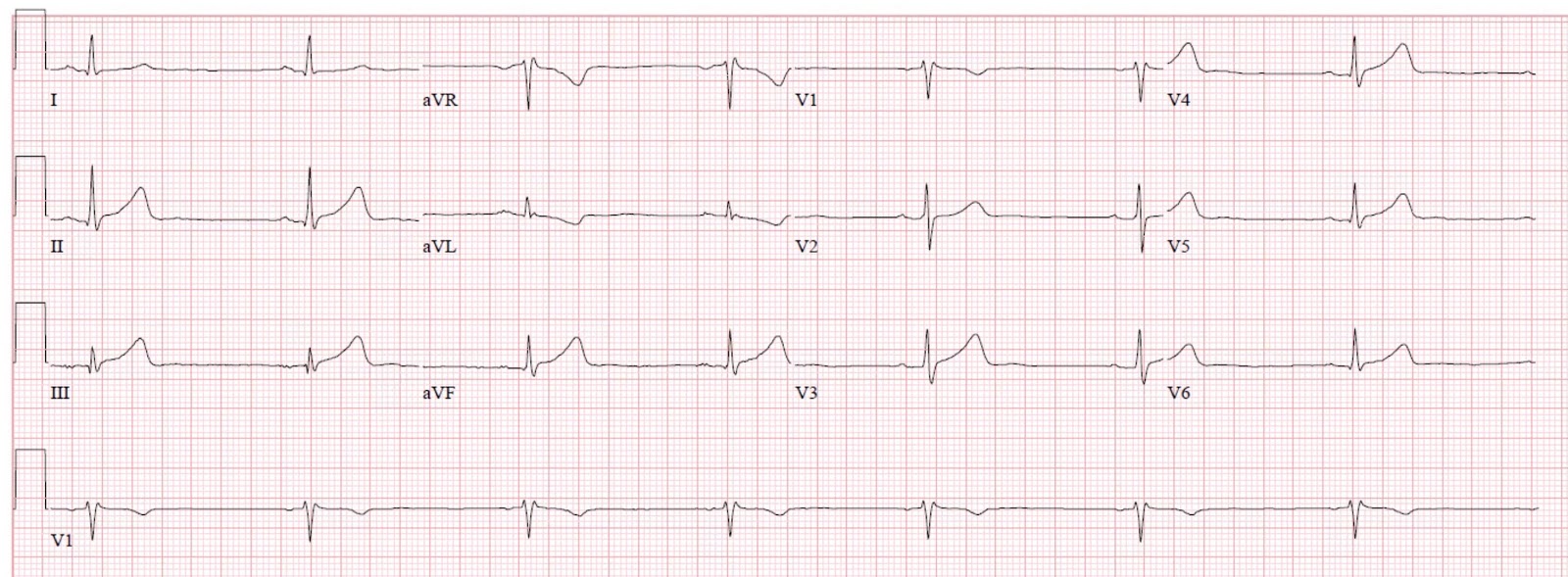
Should never and will never are different. I have not missed a STEMI but I know good docs who have, particularly inferior. When you get handed your 20th EKG in a shift where you’ve seen3 pph, I see how it can happen to a good doc.
I agree. Saying you should NEVER miss something is absurd, there is no test that is 100% sensitive and part of the reason why is human error. We all screw up at some point. There is no perfect doctor who has never missed something. Should you miss a STEMI, no you shouldnt. Can it happen when someone is handing you the 10th ecg to sign in an hour while trying to resuscitate and think about a sick crashing neonate? Absolutely. Cognitive errors happen all the time, because of constant interruptions and the other cases you have going on.