- Joined
- Dec 26, 2006
- Messages
- 7,100
- Reaction score
- 17,534
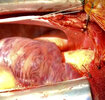
Pt is a 40 yo M, h/o of endocarditis s/p bioprosthetic MVR in 2016, PCI to RCA in 2015, aflutter, congestive hepatopathy, thrombocytopenia, recurrent pleural effusions, LAA thrombus on recent cardiac CT for which he has been on eliquis for 1 month.
He is presenting to you today for a valve-in-valve transseptal TMVR after holding his eliquis for 2 days.
You proceed with a careful induction of GETA. In this hospital cardiology does the TEE and/or TTE for cath lab procedures and here are some of the images they get:
 (CW spectral doppler is inverted here)
(CW spectral doppler is inverted here)
SPAP is 65-75 mmHg by TR CW jet
I think it’s fair to say that the LAA, despite being on eliquis for 1 mo, is still quite concerning for thrombus, and even if one isn’t going to call it frank thrombus keep mind that when doing transseptal ViV TMVR that a stiff wire frequently heads into the LAA or LUPV and does some scraping. In a 40 yo patient, the interventional cardiologists and CT surgeon were not willing to accept the stroke risk here.
So, given that A/C does not appear to be working, our only option is operative. Take note of the biventricular size and function, the appearance of the bio MVR, and the fact that the mean mitral inflow gradient (not shown) is 20 mmHg.
For residents and fellows first:
What are the echocardiographic findings in the limited images above? What interventions does this patient need? What are your preanesthetic concerns given his surgical and medical history? How are you going to induce? Which monitors and lines? How are you going to come off CPB?
He is presenting to you today for a valve-in-valve transseptal TMVR after holding his eliquis for 2 days.
You proceed with a careful induction of GETA. In this hospital cardiology does the TEE and/or TTE for cath lab procedures and here are some of the images they get:
SPAP is 65-75 mmHg by TR CW jet
I think it’s fair to say that the LAA, despite being on eliquis for 1 mo, is still quite concerning for thrombus, and even if one isn’t going to call it frank thrombus keep mind that when doing transseptal ViV TMVR that a stiff wire frequently heads into the LAA or LUPV and does some scraping. In a 40 yo patient, the interventional cardiologists and CT surgeon were not willing to accept the stroke risk here.
So, given that A/C does not appear to be working, our only option is operative. Take note of the biventricular size and function, the appearance of the bio MVR, and the fact that the mean mitral inflow gradient (not shown) is 20 mmHg.
For residents and fellows first:
What are the echocardiographic findings in the limited images above? What interventions does this patient need? What are your preanesthetic concerns given his surgical and medical history? How are you going to induce? Which monitors and lines? How are you going to come off CPB?
Last edited: