Anyone know of any research to indicate for our against giving a rate reducing rx in sinus tachycardia in the critically ill provided their BP and oxsat can handle a rate reduction?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Sinus tachycardia in critically ill : give BB/CCB?
- Thread starter 83462
- Start date
- Joined
- Jan 2, 2005
- Messages
- 504
- Reaction score
- 208
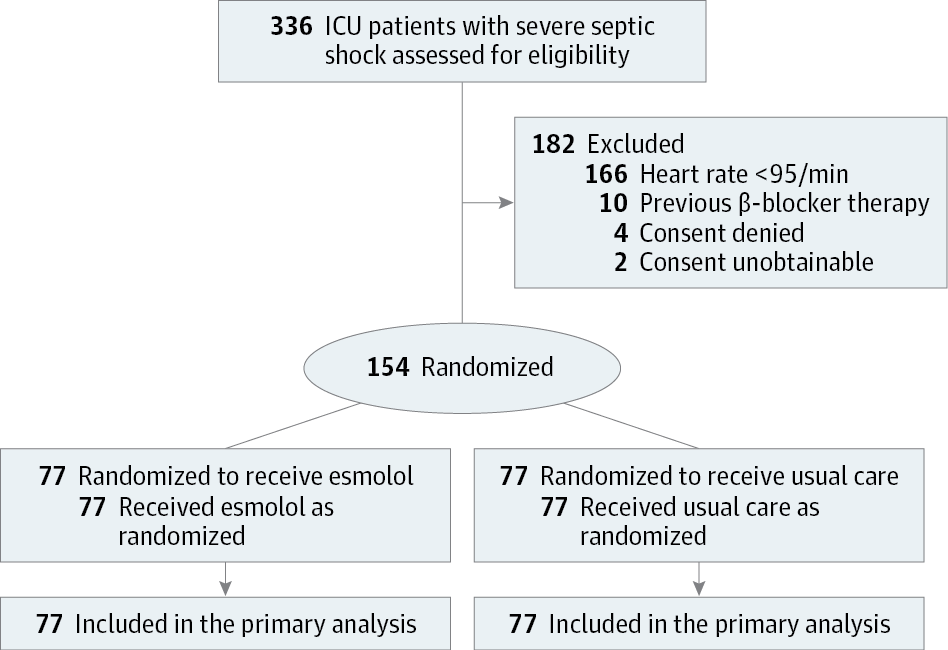
Esmolol and Heart Rate Control in Septic Shock
To determine whether treating critically ill patients with severe septic shock with esmolol, a short-acting β-blocker, to reduce their heart rates, Morelli and coauthors conducted an open-label, randomized phase 2 study, involving 154 qualifying patients treated at a university hospital intensive...
I have always found this to be an interesting line of research. Keep in mind that your mileage may vary, especially if you don't have Levosimendan to "rescue" as they put it. I think this may have more to do with blunting adrenergic effects generally than particularly preventing people from being tachycardic. Looking forward to what the CCM boarded folks post here
- Joined
- May 24, 2006
- Messages
- 6,750
- Reaction score
- 6,259
Why? Unless they are in Afib w RVR and or having a hard time filling because the HR is too high.Anyone know of any research to indicate for our against giving a rate reducing rx in sinus tachycardia in the critically ill provided their BP and oxsat can handle a rate reduction?
Fix the underlying problem. No it’s not unusual to do both a pressor and B blocker if the patient is unstable from ST.
If they are stable, why? It’s a compensatory mechanism.
How high?
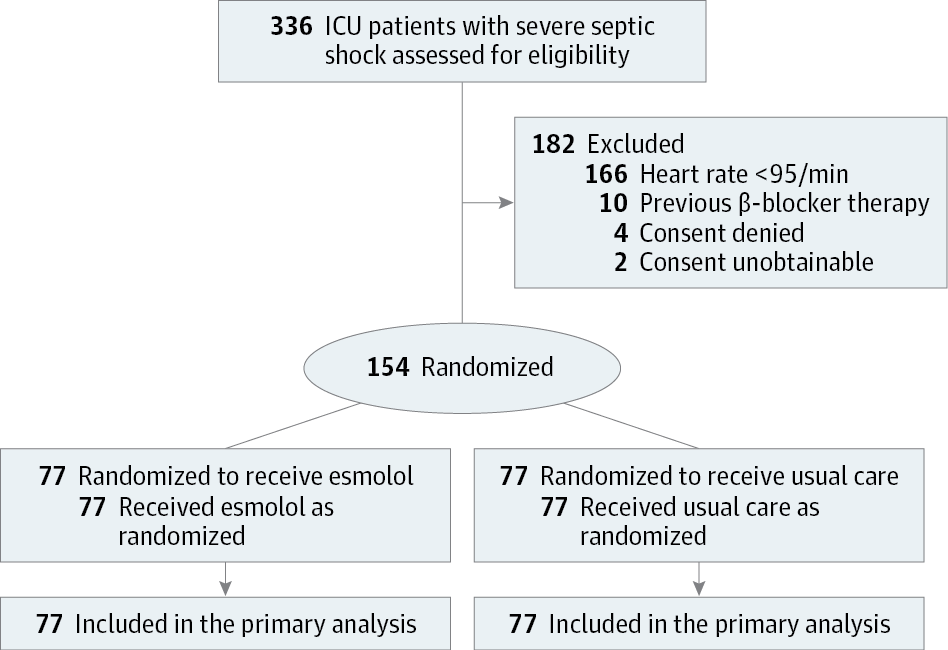
Esmolol and Heart Rate Control in Septic Shock
To determine whether treating critically ill patients with severe septic shock with esmolol, a short-acting β-blocker, to reduce their heart rates, Morelli and coauthors conducted an open-label, randomized phase 2 study, involving 154 qualifying patients treated at a university hospital intensive...jamanetwork.com
I have always found this to be an interesting line of research. Keep in mind that your mileage may vary, especially if you don't have Levosimendan to "rescue" as they put it. I think this may have more to do with blunting adrenergic effects generally than particularly preventing people from being tachycardic. Looking forward to what the CCM boarded folks post here
That study is answering a different question really. The only thing we can conclude from this is that in septic shock, AFTER 24 hours of resuscitation, in a group preselected by pulmonary artery catheterisation to have a high cardiac output and to be well resuscitated, rate control with rescue Levosimendan 50% OF THE TIME may reduce mortality. Even then the statistics don’t pass the sniff test. 80% control mortality? That isn’t usual. Maybe it was the fact that the control group was having fluid and PRBC boluses until 96 hrs into the study to maintain high CVP and PCWP and a Hb of 8 and half of that group also requiring Levosimendan. Maybe esmolol was “saving” people from crappy control management. In short this study has not changed my practice or that of anyone’s that i know.
I think you need to specify which critically ill patient group and in which stage of their illness you’re talking about because each situation is completely different.
- Joined
- Feb 27, 2015
- Messages
- 2,265
- Reaction score
- 4,222
Anyone know of any research to indicate for our against giving a rate reducing rx in sinus tachycardia in the critically ill provided their BP and oxsat can handle a rate reduction?
Sinus tachycardia with underlying cardiomyopathy (including dilated or restrictive), coronary syndromes, regurgitatant or stenotic valvulopathies, thyroid storm, sepsis -- all very different. Some I'd treat, some I'd let them tach, some need treatment but not with nodal agents. This does not include more "straightforward" cases like pulmonary embolism, hemorrhage, tamponade physiology, etc.
The evidence overall (as with most things in CCM) is sparse and treatment is based on first principles/bedside assessment of physiology. For example, diastolic filling generally doesn't become an issue until the HR > ~140 and you can assess this pretty easily on TTE (with the LVOT VTI for example).
I did a deep dive on beta-blockers for sepsis about 6 years ago on this forum. I was more convinced of the evidence when I was young and dumb. Now, I realise how tenuous all the research is -- very far away from being useful in clinical practice. There are essentially no compelling data, only "interesting" data that are not ready for prime time (with the study quoted above as a good example).
Last edited:
- Joined
- Nov 15, 2019
- Messages
- 227
- Reaction score
- 296
Had a travel RN get very upset with me for not beta blocking a DKA-er in sinus tachycardia...
Just a resident but there seems to be virtually no upside to manage sinus tachycardia acutely outside the CAD, dissection patients... just makes people feel better.
There was a time as a CA-1 where I gave esmolol instead of fentanyl for about a week before I gave up on it.
Just a resident but there seems to be virtually no upside to manage sinus tachycardia acutely outside the CAD, dissection patients... just makes people feel better.
There was a time as a CA-1 where I gave esmolol instead of fentanyl for about a week before I gave up on it.
- Joined
- Jun 9, 2016
- Messages
- 1,242
- Reaction score
- 2,209
I'd need a compelling reason to rate control sinus tachycardia (eg dissection). Unless it's IST, it's happening for a reason - target that
- Joined
- May 24, 2006
- Messages
- 6,750
- Reaction score
- 6,259
What’s IST?I'd need a compelling reason to rate control sinus tachycardia (eg dissection). Unless it's IST, it's happening for a reason - target that
- Joined
- Jun 9, 2016
- Messages
- 1,242
- Reaction score
- 2,209
What’s IST?
Inappropriate sinus tach
- Joined
- Oct 10, 2007
- Messages
- 4,253
- Reaction score
- 7,081
In sepsis (which is what the OP linked article was on) I have almost never managed sinus tachy.
IST is an outpatient diagnosisInappropriate sinus tach
their rate control is resuscitation (eg antibiotics, anticoagulation, fluids, blood, etc etc).Anyone know of any research to indicate for our against giving a rate reducing rx in sinus tachycardia in the critically ill provided their BP and oxsat can handle a rate reduction?
- Joined
- Apr 9, 2006
- Messages
- 5,439
- Reaction score
- 7,313
fluids? antibiotics? pressors? i know everyone loves levo..
phenyelphrine might help slow things down
and hey it can help with the low BP from sepsis too
phenyelphrine might help slow things down
and hey it can help with the low BP from sepsis too
- Joined
- Oct 20, 2005
- Messages
- 16,911
- Reaction score
- 47,677
My favorite part of this study: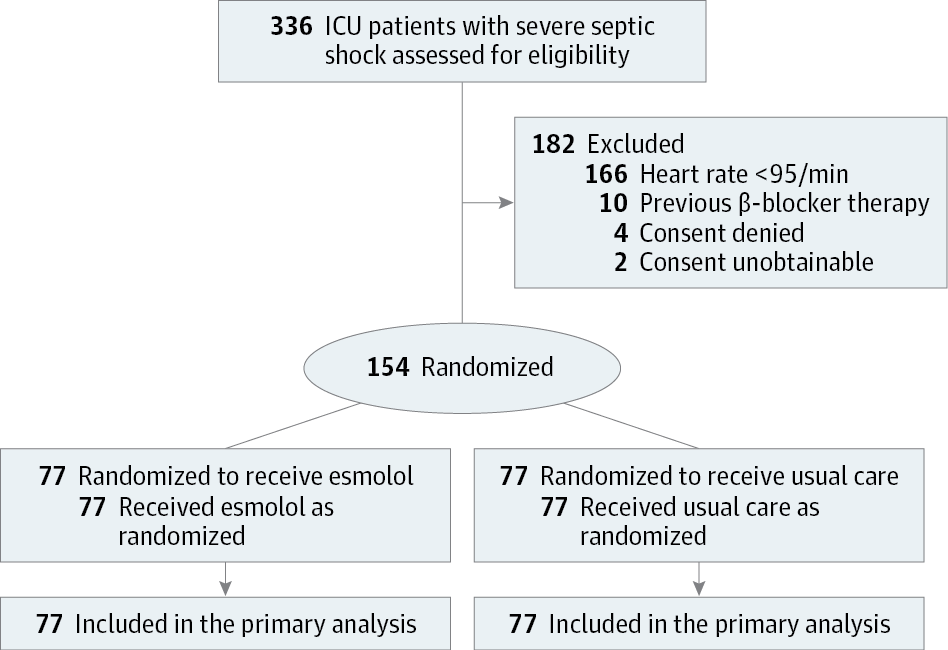
Esmolol and Heart Rate Control in Septic Shock
To determine whether treating critically ill patients with severe septic shock with esmolol, a short-acting β-blocker, to reduce their heart rates, Morelli and coauthors conducted an open-label, randomized phase 2 study, involving 154 qualifying patients treated at a university hospital intensive...jamanetwork.com
I have always found this to be an interesting line of research. Keep in mind that your mileage may vary, especially if you don't have Levosimendan to "rescue" as they put it. I think this may have more to do with blunting adrenergic effects generally than particularly preventing people from being tachycardic. Looking forward to what the CCM boarded folks post here
"Twenty-eight day mortality was... 80.5% in the control group"
It appears the control arm treatment was a gunshot to the head.
- Joined
- Sep 17, 2016
- Messages
- 778
- Reaction score
- 1,251
I’ll treat sinus tach so the surgeon feels comfortable with the patient going to the floor from SICU...
D
deleted547339
I’ll treat sinus tach so the surgeon feels comfortable with the patient going to the floor from SICU...
That sounds like a bad idea....
- Joined
- Sep 17, 2016
- Messages
- 778
- Reaction score
- 1,251
Agreed. The number of times I’ve had to treat a number just to get a patient out of SICU is too gosh darn high!That sounds like a bad idea....
I've seen a few mortalities from beta blocking sinus tach. Depending on the underlying cause, ST can be a response to low cardiac output. Blocking this backup defensive mechanism can suddenly drop CO with resultant cardiac arrest. Especially problematic in PE, cardiogenic shock, tamponade, PTX, hypovolemia etc.
Find the underlying cause and treat if possible. Otherwise leave it alone unless patient is dependent on diastolic filing time.
Find the underlying cause and treat if possible. Otherwise leave it alone unless patient is dependent on diastolic filing time.
- Joined
- Jun 9, 2016
- Messages
- 1,242
- Reaction score
- 2,209
I've seen a few mortalities from beta blocking sinus tach. Depending on the underlying cause, ST can be a response to low cardiac output. Blocking this backup defensive mechanism can suddenly drop CO with resultant cardiac arrest. Especially problematic in PE, cardiogenic shock, tamponade, PTX, hypovolemia etc.
Find the underlying cause and treat if possible. Otherwise leave it alone unless patient is dependent on diastolic filing time.
It's the worst in little kids that can't modulate their SV much. Someone unfamiliar with kids sees a HR of 200 and uses an AVNB, womp womp
- Joined
- Jan 2, 2005
- Messages
- 504
- Reaction score
- 208

Effect of Ultrashort-Acting β-Blockers on Mortality in Patients With Sepsis With Persistent Tachycardia Despite Initial Resuscitation: A Systematic Review and Meta-analysis of Randomized Controlled Trials - PubMed
UMIN Clinical Trials Registry; No.: UMIN000040174; URL: https://www.umin.ac.jp/ctr/index.htm.
More evidence on this topic, a meta-analysis of seven RCTs with a pooled sample size of 613 patients. I don't disagree with anything anyone wrote in response to the earlier paper I posted, but it's an interesting question I think -- perhaps there is benefit in modulating adrenergic tone after appropriate resuscitation, maybe it's just the heart, maybe it's something else. Not something I intend on incorporating into my practice, but I think it's cool to think about the potential mechanisms.
- Joined
- Oct 20, 2005
- Messages
- 16,911
- Reaction score
- 47,677
It makes me slightly worried that more that half the articles aren't in English, not that good studies can't be done in other countries, but there clearly was a reason they didn't publish in an English speaking journal given the ubiquitous access to language services for publications nowadays. The lack of clear data on baseline characteristics makes it also challenging to interpret. I mean, Dopamine used be a front-line agent for sepsis, but fell out of favor in adults (then pediatrics) related to the tachyarrhythmias it induced. If you're septic and prone to a tachyarrhythmia, could rate control actually be helpful? I mean, it seems like the answer would be yes. I suspect that is what they are seeing (in fact, that's what the Lancet Resp. Med article shows). Now, does that mean it should be extrapolated to every patient with tachycardia irrespective of their arrhythmia risk? I would guess no. But I say that knowing that we give out Propranolol like water to burn patients because of perceived inappropriate tachycardia. Of course, the effect on outcomes isn't mortality but visceral fat, but is there a role for short acting B-blockade? Maybe. Clearly this question needs to be answered in a better fashion.
Effect of Ultrashort-Acting β-Blockers on Mortality in Patients With Sepsis With Persistent Tachycardia Despite Initial Resuscitation: A Systematic Review and Meta-analysis of Randomized Controlled Trials - PubMed
UMIN Clinical Trials Registry; No.: UMIN000040174; URL: https://www.umin.ac.jp/ctr/index.htm.pubmed.ncbi.nlm.nih.gov
More evidence on this topic, a meta-analysis of seven RCTs with a pooled sample size of 613 patients. I don't disagree with anything anyone wrote in response to the earlier paper I posted, but it's an interesting question I think -- perhaps there is benefit in modulating adrenergic tone after appropriate resuscitation, maybe it's just the heart, maybe it's something else. Not something I intend on incorporating into my practice, but I think it's cool to think about the potential mechanisms.
beta blocker plus dopamine is just phenylepi in a roundabout wayIt makes me slightly worried that more that half the articles aren't in English, not that good studies can't be done in other countries, but there clearly was a reason they didn't publish in an English speaking journal given the ubiquitous access to language services for publications nowadays. The lack of clear data on baseline characteristics makes it also challenging to interpret. I mean, Dopamine used be a front-line agent for sepsis, but fell out of favor in adults (then pediatrics) related to the tachyarrhythmias it induced. If you're septic and prone to a tachyarrhythmia, could rate control actually be helpful? I mean, it seems like the answer would be yes. I suspect that is what they are seeing (in fact, that's what the Lancet Resp. Med article shows). Now, does that mean it should be extrapolated to every patient with tachycardia irrespective of their arrhythmia risk? I would guess no. But I say that knowing that we give out Propranolol like water to burn patients because of perceived inappropriate tachycardia. Of course, the effect on outcomes isn't mortality but visceral fat, but is there a role for short acting B-blockade? Maybe. Clearly this question needs to be answered in a better fashion.
- Joined
- May 24, 2006
- Messages
- 6,750
- Reaction score
- 6,259
Funny you should mention this. When I was a bit of a newbie I had a septic patient with Afib RVR that I was giving Norepi and lots of fluid to in the OR. Had to be perforated viscus or something like it. I gave lots of fluid as source control was happening but, I couldn't slow the rate down. I remember texting my partner about either the surgeon or RN suggesting a beta blocker, but of course, I declined knowing that if I fixed the acidosis I would fix the problem. My 65 year old partner said, "well a beta blocker isn't a contraindication in case like this". Of course I never did as I texted after the fact and I don't remember what happened to the patient.It makes me slightly worried that more that half the articles aren't in English, not that good studies can't be done in other countries, but there clearly was a reason they didn't publish in an English speaking journal given the ubiquitous access to language services for publications nowadays. The lack of clear data on baseline characteristics makes it also challenging to interpret. I mean, Dopamine used be a front-line agent for sepsis, but fell out of favor in adults (then pediatrics) related to the tachyarrhythmias it induced. If you're septic and prone to a tachyarrhythmia, could rate control actually be helpful? I mean, it seems like the answer would be yes. I suspect that is what they are seeing (in fact, that's what the Lancet Resp. Med article shows). Now, does that mean it should be extrapolated to every patient with tachycardia irrespective of their arrhythmia risk? I would guess no. But I say that knowing that we give out Propranolol like water to burn patients because of perceived inappropriate tachycardia. Of course, the effect on outcomes isn't mortality but visceral fat, but is there a role for short acting B-blockade? Maybe. Clearly this question needs to be answered in a better fashion.
All this to say that yea, in certain instances, like the article says, once you have fluid rescusicated enough, you can try to rate control w a beta blocker along w pressor to improve CO. I now know better of course and of course I looked it up right then after texting my colleague and thought I should have given the esmolol after all.
