- Joined
- Jan 18, 2013
- Messages
- 152
- Reaction score
- 15
young female, known to have a metastatic breast cancer, since 5 years.
In 2017, she developed secondary lesions in the brain with positive CSF.
She receives 30Gy/10 fr whole brain radiation, with intra-thecal chemotherapy.
A month ago, she developed gait disturbances with blurred speech an hemifacial paresia.
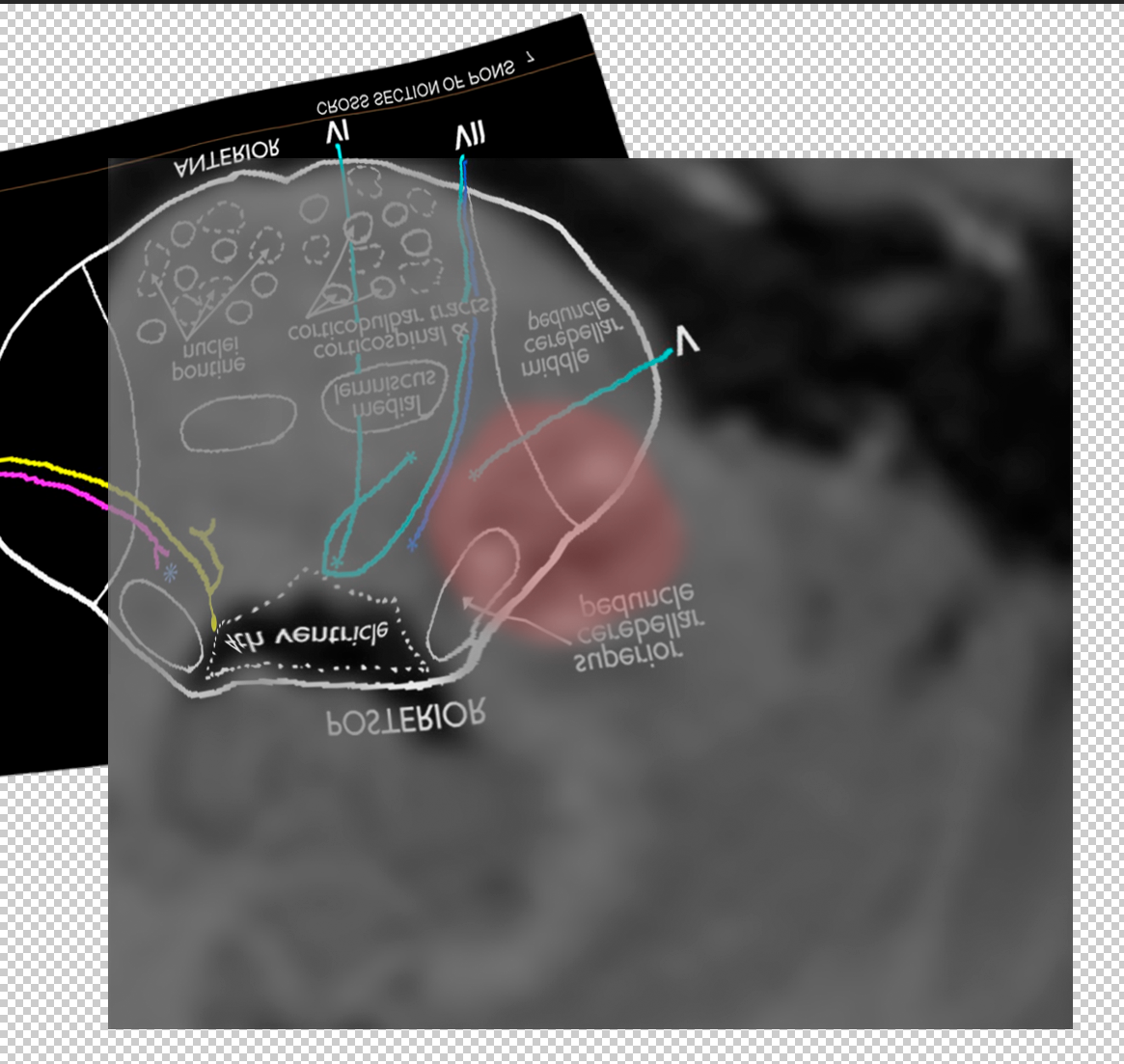
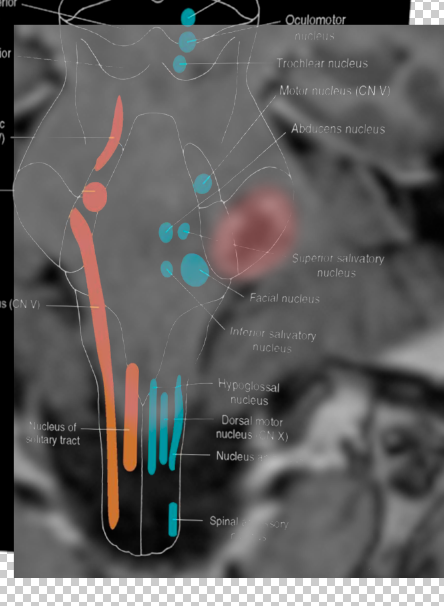
Brain MRI showed a solitary secondary lesion, 1.5 cm involving the left middle cerebral peduncle with extensive edema. No signs of meningeal disease.
Pet CT : NED outside the brain.
She was referred for brain SRS.
I need your advice concerning the dose and fractionation SRS vs FSRT, noting the close proximity of the BS and the Hx of Brain RT.
In 2017, she developed secondary lesions in the brain with positive CSF.
She receives 30Gy/10 fr whole brain radiation, with intra-thecal chemotherapy.
A month ago, she developed gait disturbances with blurred speech an hemifacial paresia.
Brain MRI showed a solitary secondary lesion, 1.5 cm involving the left middle cerebral peduncle with extensive edema. No signs of meningeal disease.
Pet CT : NED outside the brain.
She was referred for brain SRS.
I need your advice concerning the dose and fractionation SRS vs FSRT, noting the close proximity of the BS and the Hx of Brain RT.