- Joined
- Aug 22, 2008
- Messages
- 195
- Reaction score
- 0
A Life-Changing Case for Doctors in Training
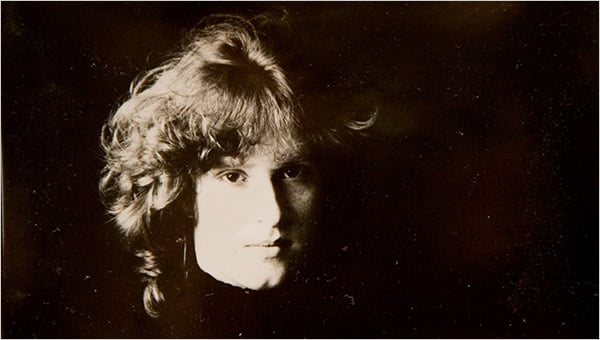 A DAUGHTER LOST After Libby Zion died in a hospital at age 18, her fathers crusade led to changes in work hours and supervision of medical residents.
A DAUGHTER LOST After Libby Zion died in a hospital at age 18, her fathers crusade led to changes in work hours and supervision of medical residents.
By BARRON H. LERNER, M.D.
Published: March 2, 2009
Doctor and Patient: On Young Doctors and Long Workdays (March 3, 2009)
The efforts of her bereaved and furious father, Sidney Zion, set into a motion a series of reforms to the system of medical education that he believed had killed his daughter.
I remember the Zion case vividly because I was a medical student when Libby died. To this day, especially among students and physicians practicing medicine in New York at the time, the case inspires intense emotions and impassioned arguments.
The exact cause of Libbys death was never found, but many facts are known. When she was admitted to New York Hospital (now New York Presbyterian Hospital) on the evening of March 4, 1984, she was an 18-year-old college freshman with a high fever and mysterious jerking movements. She was alternately cooperative and agitated. She had a history of depression and was taking phenelzine, an antidepressant.
The physicians admitted Libby for observation and hydration, suspecting she had a viral syndrome. She was also given meperidine, an opiate drug used to stop shaking movements. The physicians who evaluated her doctors in training known as residents touched base with Dr. Raymond Sherman, the Zions family doctor and the attending physician of record, who agreed with the plan. It was about 3 a.m. on March 5.
But Libby became more agitated. When notified of this, the first-year resident who had evaluated her, Dr. Luise L. Weinstein, ordered physical restraints as well as a shot of haloperidol, another sedating medication. Busy covering dozens of other patients, Dr. Weinstein did not visually evaluate Libby again. The second-year resident on the case, Dr. Gregg Stone, had gone across the street to try to get a few hours of sleep, as was customary at the time.
The nurses later reported that Libby finally calmed down, but when her vital signs were rechecked at 6 that morning, her temperature was an alarming 107 degrees. The staff immediately tried to cool her. But she soon suffered a cardiac arrest, and despite extensive attempts at resuscitation, she could not be brought back.
After their initial grief and shock, Sidney Zion and his wife, Elsa, hired a lawyer and began to investigate Libbys death. When Mr. Zion learned that his daughter had been tied down and not re-evaluated, that the only doctors who had seen her were in training, that such doctors routinely worked 36-hour shifts with little or no sleep, and that the attending physician had never come into the hospital, his response turned to fury.
He decided to make his daughters death a crusade for reform. A former lawyer and a powerful journalist who had worked for The New York Times and other newspapers, he enlisted fellow reporters across the country to tell his daughters story. He even persuaded the Manhattan district attorney, Robert M. Morgenthau, to take the highly unusual step of convening a grand jury to consider murder charges against the physicians involved.
At the Columbia College of Physicians and Surgeons, my fellow medical students and I replayed the events of that night. Would we have ordered restraints and not seen her? Would we have sent her to the intensive care unit? Would we have known about a potentially toxic interaction between the drugs in her body?
Ultimately, we concluded that there but for the grace of God go I. We could not definitively state that we would have done anything differently. The young doctors caring for Libby Zion had been in the wrong place at the wrong time. When I subsequently had the opportunity to research the case for a book on famous patients, I concluded that the admitting team had a good plan but had erred in not realizing that their patients condition was deteriorating.
The malpractice case, which went to trial in 1994, ultimately assigned equal blame to New York Hospital and Libby Zion for supposedly concealing her past use of cocaine. But the cases real legacies were the issues of resident work hours and supervision.
This came as no surprise to those of us in the trenches. We knew what it was like to stay up for 36 hours straight, first as medical students and later as residents. It was, in a word, insanity. Deprived of sleep, we roamed the wards, dreaming of when we could finally leave, dozing off on rounds, screaming at patients and colleagues and praying we would not make any grievous mistakes. As Sidney Zions campaign took off, I felt sorry for the competent and well-meaning doctors he pilloried, but was thrilled that change was occurring.
The impetus for reform was the grand jury, which did not indict the physicians but rather issued a report highly critical of the hospital. This led to the formation of a state commission, headed by the New York physician Dr. Bertrand Bell, which in 1987 recommended that doctors in training work no more than 80 hours a week and no more than 24 hours in a row and receive significantly more on-site supervision from senior physicians. In 2003, the Accreditation Council for Graduate Medical Education made these recommendations mandatory for all residency training programs.
But this was not enough. This past December, the Institute of Medicine released a report recommending even stricter work-hour reductions and concluding that supervision of young physicians remained inadequate.
It had taken 25 years, but Sidney Zions dream had been realized at least in part. In a recent interview, he told me he hoped that financing would be forthcoming to carry out the reforms. I dont know anyone who still works 24 straight hours in any other business, he said. And these are people with lives in their hands.
The changes do have their critics, who say that night float systems, put into place to allow residents to sleep, make patient care disjointed, producing shift worker doctors who never truly learn how complicated illnesses evolve in the first crucial 24 to 36 hours. A 2007 study in The Archives of Internal Medicine, for example, revealed high rates of errors resulting from poor handoffs of information between physicians.
The Institute of Medicine report does not ignore these concerns and makes suggestions for improving the new systems. But thinking back to those days and nights throwing back cups of coffee to barely stay awake, I know we cannot afford to turn back. When I now work with well-rested, pleasant and enthusiastic residents, my thoughts turn to Libby Zion. Her fathers cause, at least, is alive and well.
Barron H. Lerner, a professor of medicine and public health at Columbia University Medical Center, is the author of When Illness Goes Public: Celebrity Patients and How We Look at Medicine.
- Prin
By BARRON H. LERNER, M.D.
Published: March 2, 2009
Doctor and Patient: On Young Doctors and Long Workdays (March 3, 2009)
The efforts of her bereaved and furious father, Sidney Zion, set into a motion a series of reforms to the system of medical education that he believed had killed his daughter.
I remember the Zion case vividly because I was a medical student when Libby died. To this day, especially among students and physicians practicing medicine in New York at the time, the case inspires intense emotions and impassioned arguments.
The exact cause of Libbys death was never found, but many facts are known. When she was admitted to New York Hospital (now New York Presbyterian Hospital) on the evening of March 4, 1984, she was an 18-year-old college freshman with a high fever and mysterious jerking movements. She was alternately cooperative and agitated. She had a history of depression and was taking phenelzine, an antidepressant.
The physicians admitted Libby for observation and hydration, suspecting she had a viral syndrome. She was also given meperidine, an opiate drug used to stop shaking movements. The physicians who evaluated her doctors in training known as residents touched base with Dr. Raymond Sherman, the Zions family doctor and the attending physician of record, who agreed with the plan. It was about 3 a.m. on March 5.
But Libby became more agitated. When notified of this, the first-year resident who had evaluated her, Dr. Luise L. Weinstein, ordered physical restraints as well as a shot of haloperidol, another sedating medication. Busy covering dozens of other patients, Dr. Weinstein did not visually evaluate Libby again. The second-year resident on the case, Dr. Gregg Stone, had gone across the street to try to get a few hours of sleep, as was customary at the time.
The nurses later reported that Libby finally calmed down, but when her vital signs were rechecked at 6 that morning, her temperature was an alarming 107 degrees. The staff immediately tried to cool her. But she soon suffered a cardiac arrest, and despite extensive attempts at resuscitation, she could not be brought back.
After their initial grief and shock, Sidney Zion and his wife, Elsa, hired a lawyer and began to investigate Libbys death. When Mr. Zion learned that his daughter had been tied down and not re-evaluated, that the only doctors who had seen her were in training, that such doctors routinely worked 36-hour shifts with little or no sleep, and that the attending physician had never come into the hospital, his response turned to fury.
He decided to make his daughters death a crusade for reform. A former lawyer and a powerful journalist who had worked for The New York Times and other newspapers, he enlisted fellow reporters across the country to tell his daughters story. He even persuaded the Manhattan district attorney, Robert M. Morgenthau, to take the highly unusual step of convening a grand jury to consider murder charges against the physicians involved.
At the Columbia College of Physicians and Surgeons, my fellow medical students and I replayed the events of that night. Would we have ordered restraints and not seen her? Would we have sent her to the intensive care unit? Would we have known about a potentially toxic interaction between the drugs in her body?
Ultimately, we concluded that there but for the grace of God go I. We could not definitively state that we would have done anything differently. The young doctors caring for Libby Zion had been in the wrong place at the wrong time. When I subsequently had the opportunity to research the case for a book on famous patients, I concluded that the admitting team had a good plan but had erred in not realizing that their patients condition was deteriorating.
The malpractice case, which went to trial in 1994, ultimately assigned equal blame to New York Hospital and Libby Zion for supposedly concealing her past use of cocaine. But the cases real legacies were the issues of resident work hours and supervision.
This came as no surprise to those of us in the trenches. We knew what it was like to stay up for 36 hours straight, first as medical students and later as residents. It was, in a word, insanity. Deprived of sleep, we roamed the wards, dreaming of when we could finally leave, dozing off on rounds, screaming at patients and colleagues and praying we would not make any grievous mistakes. As Sidney Zions campaign took off, I felt sorry for the competent and well-meaning doctors he pilloried, but was thrilled that change was occurring.
The impetus for reform was the grand jury, which did not indict the physicians but rather issued a report highly critical of the hospital. This led to the formation of a state commission, headed by the New York physician Dr. Bertrand Bell, which in 1987 recommended that doctors in training work no more than 80 hours a week and no more than 24 hours in a row and receive significantly more on-site supervision from senior physicians. In 2003, the Accreditation Council for Graduate Medical Education made these recommendations mandatory for all residency training programs.
But this was not enough. This past December, the Institute of Medicine released a report recommending even stricter work-hour reductions and concluding that supervision of young physicians remained inadequate.
It had taken 25 years, but Sidney Zions dream had been realized at least in part. In a recent interview, he told me he hoped that financing would be forthcoming to carry out the reforms. I dont know anyone who still works 24 straight hours in any other business, he said. And these are people with lives in their hands.
The changes do have their critics, who say that night float systems, put into place to allow residents to sleep, make patient care disjointed, producing shift worker doctors who never truly learn how complicated illnesses evolve in the first crucial 24 to 36 hours. A 2007 study in The Archives of Internal Medicine, for example, revealed high rates of errors resulting from poor handoffs of information between physicians.
The Institute of Medicine report does not ignore these concerns and makes suggestions for improving the new systems. But thinking back to those days and nights throwing back cups of coffee to barely stay awake, I know we cannot afford to turn back. When I now work with well-rested, pleasant and enthusiastic residents, my thoughts turn to Libby Zion. Her fathers cause, at least, is alive and well.
Barron H. Lerner, a professor of medicine and public health at Columbia University Medical Center, is the author of When Illness Goes Public: Celebrity Patients and How We Look at Medicine.

 You choose the right specialty to apply to then.
You choose the right specialty to apply to then.