- Joined
- Jul 6, 2004
- Messages
- 1,977
- Reaction score
- 563
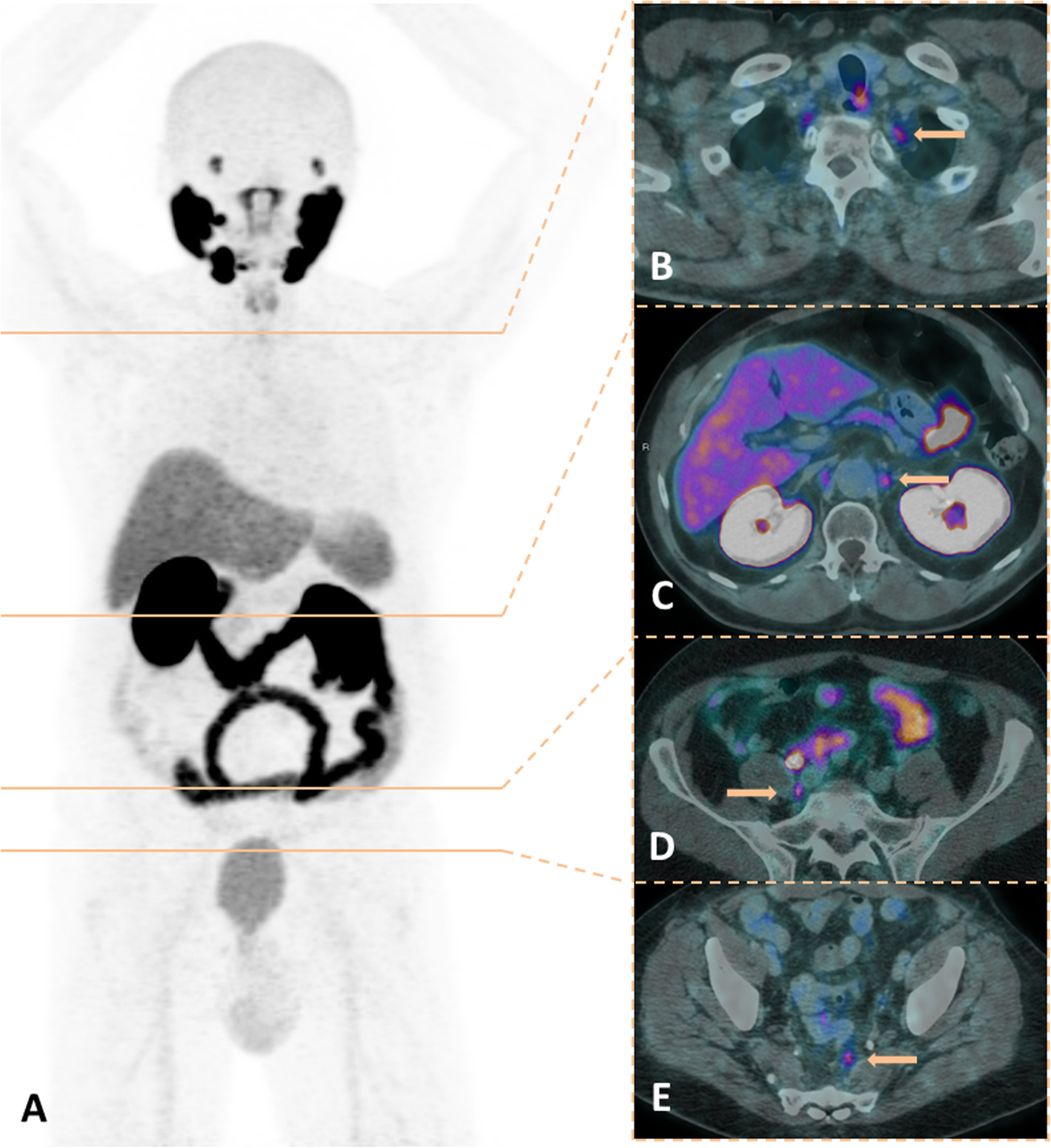
53 yo very healthy man with unfav int risk prostate cancer Gleason 4+3 in 12 of 16 targeted biopsy cores PSA 16 ng/ml (was 14 back in November) had a PSMA for staging that shows Suvmax uptake of 4.1 in a small perirectal node (see picture). There was an MRI done prior to the PSMA that shows a very small node there (wasnt called on the MRI read bc it was so small). Patient pretty interested in surgery but surgery did refer to us for discussion first and also noted in tumor board that they likely can not get to the node. Just curious what people think. Looks like an unusual spot for prostate met too, its pretty posterior to the external iliac on the left that I dont think it would have gotten good coverage with standard volumes