- Joined
- Jun 20, 2005
- Messages
- 8,022
- Reaction score
- 2,815
Try it on your next carotid and let me know if you notice a difference.
No. It's an EEG monitor compiled into a number. I really don't expect it to be sensitive enough to detect early ischemia. They would have advertised the hell out of that.Here's a question for you smart guys. Can you use a BIS as a cerebral oximetry monitor?
It's not extremely accurate but you will notice change if ischemia begins.No. It's an EEG monitor compiled into a number. I really don't expect it to be sensitive enough to detect early ischemia. They would have advertised the hell out of that.
This, no narc GA w sevo no ponv.Preop - 2mg midaz --> block
Intraop - general
Postop - patient goes home pain free
As one who rarely manages patients in beach chair positioning, how often are you regulars seeing/managing Bezold-Jarisch reflex manifestations? What is your most effective management?
.
I don't buy the nsaid will reduce post-op swelling.

Makes sense to me, too. You get the anti-inflammatory effects of COX-2, without the antiaggregant effects of COX-1.
On the other hand, we give 4-8 mg of decadron to many of our patients, to prevent PONV, so giving the COX-2 inhibitor too sounds superfluous.
That's fine. But, you need to clarify where you are monitoring the BP.
Anectodal, but back in the day, when we had 20-30 post-op blocks to round on, it was pretty evident that those who recieved the pill cocktail in addition to PNB did much better than those who did not. Especially if kept on a regimen for the first 3 days.
Why is the block business drying up?
That's fine. But, you need to clarify where you are monitoring the BP.

I do too. I give ketorolac in preop holding more often than I give midazolam ... then 5 minutes before closing when the surgeon magnanimously leans over and says "you can give Toradol" I just smile and nod.I do:
Having Cox-2 inhibition before mechanical trauma is beneficial. Decreasing inducible prostaglandins is a good thing... decreases vascular permeability and edema.
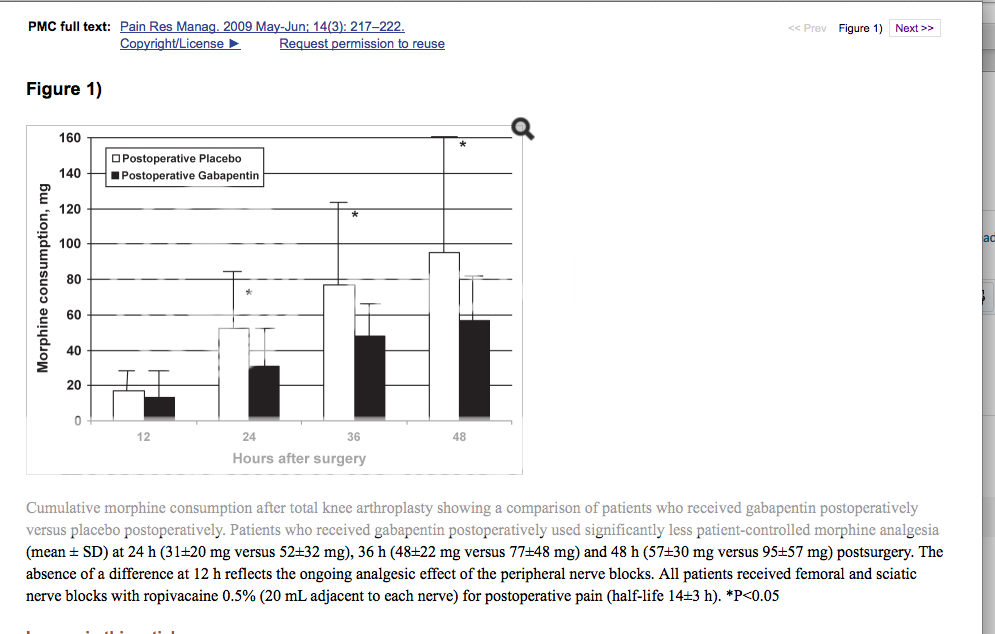
And what do COX-2 inhibitors do, according to your own figure?Different mechanisms. Decadron inhibits the synthesis of prostaglandins.
And what do COX-2 inhibitors do, according to your own figure?
Different mechanisms. Decadron inhibits the synthesis of prostaglandins.
Do you?
When patients go to their doctor's clinic, or sit in the chair at Wal-Mart, where are they monitoring the BP? The arm. Are they sitting? Yes.
When they check in to day surgery, where does the baseline BP get measured? The arm. Are they sitting? Yes.
What's so special about sitting in the OR and getting the BP measured on the arm? Nothing.
Volatiles reduce CMRO2 and impair autoregulation (causing cerebral vasodilationwhich would increase flow at a given pressure).My still-a-resident thought is that the difference is due to the altered cerebral autoregulation with inhaled anesthetics and propofol making them more pressure-dependent.
Umm...don't NSAIDs do that?
ETA: Someone beat me to it.
And what do COX-2 inhibitors do, according to your own figure?
Well in that case:and I raise you a
...!

Drastic overkill with oximetry monitoring in my opinion. The twin statements of "there is little evidence" AND "I'll keep using it on the off chance that I get sued" completely undermines the argument for its use.
I hope that the anaesthetic trainees are listening closely to the rationale discussed by the various seniors. It actually matters little what you use, but more that you have thought about it and made a justifiable choice based on experience, evidence and social justice (i.e. equitable distribution of health care assists).
Put it on the arm as usual. You know the brain is like 20 points lower.
My guess is that the 4 patients who had the infamous stroke were run at MAPs of 60 to 70 monitored on the arm. The brain was fairly hypotensive. Who knows if they were hyperventilated also?
I'm not saying that cerebral oximetry does not make sense from a scientific standpoint. My point is that the number needed to treat times the price of the device does not factor favorably against the root of the problem.
What do you mean by adding 15 to the MAP?I think an a-line is overkill in beachchair position. Just take the BP frequently and add 15 to the MAP.
I don't have the luxury of ASA 1-2 patients; or, the Ferris Doctrine to insulate me from lawsuits.


Surely that's directed at me.
Just to clear up a point of fact, the broad medicolegal protection afforded by Feres Doctrine only applies to patients presently on active duty. I'm not sure I've ever cared for a middle-aged to elderly chronically bad HTN patient ... still in uniform. In fact, the overwhelming majority of patients cared for at military hospitals are retirees and retirees' spouses, and the spouses and kids of active duty personnel, and they can and do sue. So that whole "can't sue" thing is a little overstated. (What I do have going for me is that they have to sue the government and not me directly, and my liability "policy" has the deepest of deep pockets. And I think that's a pretty awesome perk of my otherwise underpaying employer.)
Regardless. There's defensive medicine, and then there's arterial lines and cerebral oximetry for sitting shoulders. I am not by any means reluctant to place an a-line in anyone who has an indication, to wit, potential for harm from possible abrupt derangements in BP that would be missed by a q3min cuff, inability to obtain reliable NIBPs because of BMI-induced conical arms, etc.
But there ain't nothin' wrong or risky about using "just" a BP cuff in a chronic hypertensive patient sitting for a shoulder surgery if you keep their pressures near baseline, and obfuscating this issue with defensive statements about how you don't want to get sued doesn't change that.
Now, obviously if you let them ride with maps 40% below baseline because the orthopod asked you to make his patient bleed less and you agreed, you're asking for it and your monitor of choice makes no difference in the matter.
What do you mean by adding 15 to the MAP?
I think he means subtract.
Another key point here is WHO is actually sitting the case? Monitors don't save lives but they do make it easier for certain groups of providers to pay close attention to details.
I don't use anything other than a BP cuff on the arm for 50% of my beach chair cases. The other 25% get arterial lines and the last group gets Arterial line plus Cerebral Oximetry. Again, monitors don't make up for lack of vigilance but they do help reinforce the issue to pay attention to the vitals and NO MATH is required or cycling of the cuff.
I usually try to adapt to the surgical technique, instead of the other way round, but beach chair shoulders should go the way of cataract surgeries with GA or retrobulbar block. Seriously, this is 2014. Why put the patient at risk, just because the surgeon is incompetent, and has been doing things the same way for decades? Anything that can be done in lateral position should not be done in prone or beach chair, and this should be a hospital rule.Having said that, we have three surgeons who routinely do shoulders. Two do them in beach chair. The other one does them in lateral supine with suspension. Have yet to have a catastrophic anoxic event. The majority just get the standard BP cuff.