- Joined
- May 3, 2017
- Messages
- 333
- Reaction score
- 431
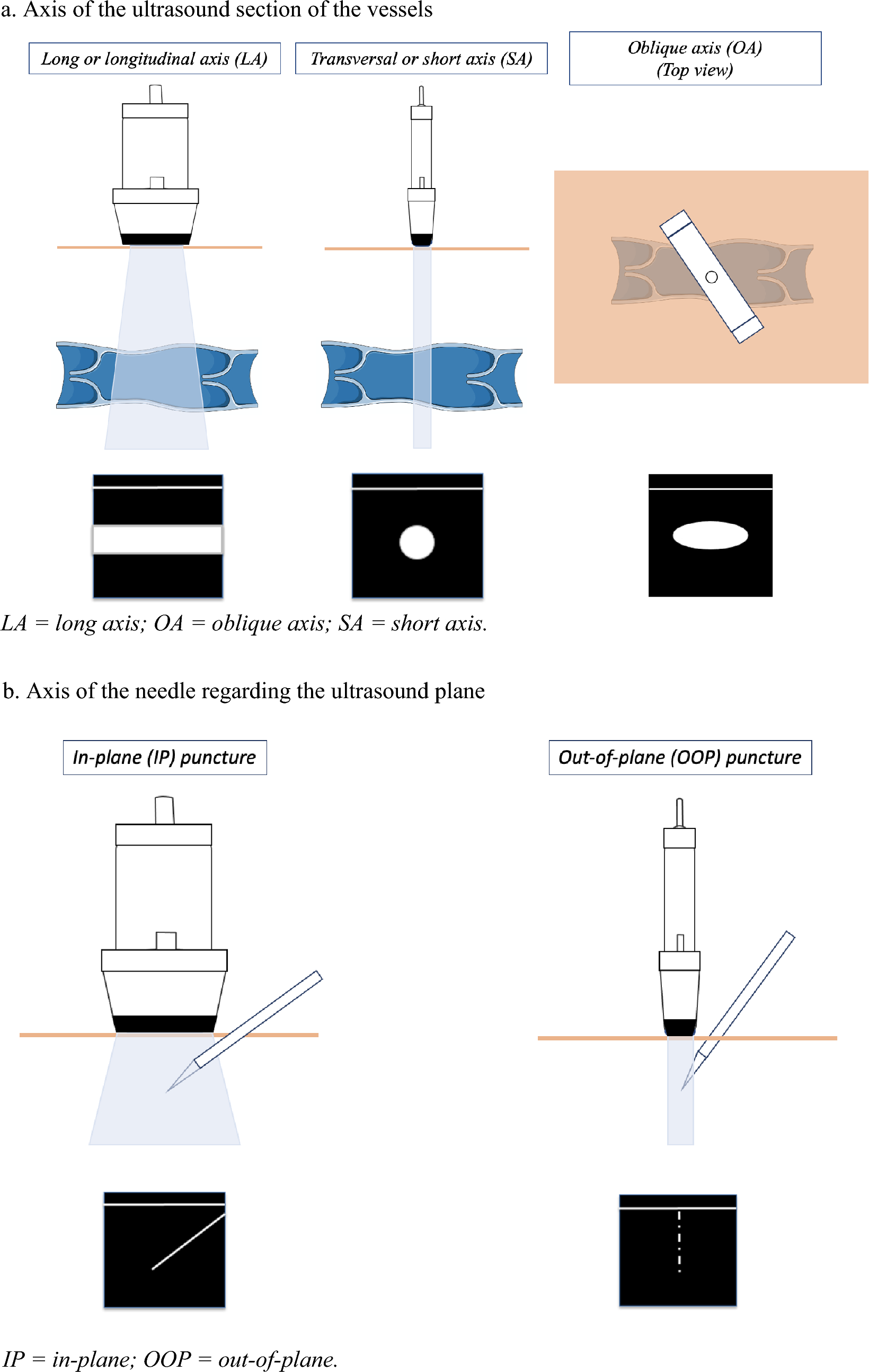
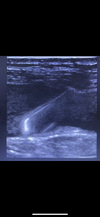
Do any of you guys do in plane for visualizing the needle and IJ when placing central line ? I’m just curious as I’ve never placed one this way but something I’m interested in. Anything you have to do differently especially when making the skin nick and threading the wire ?