- Joined
- Jun 24, 2019
- Messages
- 791
- Reaction score
- 885
Thoughts, seen this at your practice? Believe the sequalae can be worse than this?
Thoughts, seen this at your practice? Believe the sequalae can be worse than this?
Long-Covid. It’s the next line item that you’ll be adding to “24 year old female with a pmhx of anxiety, borderline, EDS, POTS, chronic Lyme....”
Elaborate on what you think that is. PEs? Pulmonary fibrosis? "Chronic fatigue"? I need a headline syndrome?
Yeah but how much is psychosomatic? Do they actually have measurable differences in their PFTs? VO2max? Fibrosis on CT? Bronchiectasis? Why are these people in the ER again? New process? You're going to of course see people thriving on a possible "post covid syndrome" for sympathy, attention, Instagram likes, etc. Most normal people go back to their normal lives.Yes I’ve had patients with this.
Abnormal vital signs have matched up with their complaints. More tachycardic than usual, lower 02 sat. Nothing life threatening but definitely not back to baseline for a month plus.
A lot of ongoing headaches. Also, general feeling of shortness of breath, like after just walking a block or 2. I hear that more from people who used to be active exercisers/runners.
I’ve personally never seen this with the flu in younger patients under 50 like I have with Covid, but maybe patients just aren’t reporting it?
Will be interesting to see what the actual long term course will be a year+ out.
Yeah but how much is psychosomatic? Do they actually have measurable differences in their PFTs? VO2max? Fibrosis on CT? Bronchiectasis? Why are these people in the ER again? New process? You're going to of course see people thriving on a possible "post covid syndrome" for sympathy, attention, Instagram likes, etc. Most normal people go back to their normal lives.
I see a TON of Covid and I don't really see any sequelae overall. I see some PEs, but almost always the 2 week mark which I don't consider non acute phase. Even then it's significantly less VTE than docs/media are making it out to be. We essentially decreased the amount of CTAs we are doing significantly because they're pointless unless clinical irregularities like hypoxia without CXR changes, profound tachycardia, etc.
The exception is chronically ill LTC patients. Most of these patients are screwed up bad post covid. Almost always have multiple lab abnormalities, mental status changes, new infections, etc
Tens of millions of people have had COVID at this point. It's unavoidable that a portion of those will have some long term effects that are real. It's equally unavoidable, that a portion of those tens of millions will blame symptoms unrelated to COVID, on their past COVID. Every generation needs it's "mitral valve prolapse," or "chronic fatigue syndrome" on which to blame all of their unrelated ills and personal deficiencies. Something was going to come along and replace "gluten" as the source of all our ills. This year it happens to be "long COVID." Next year it will be something else.
The Sleep Number Burger!My all-time favorite was a couple who wanted to split a hamburger; but ordered each half at two different temps (medium, and well).
The Sleep Number Burger!
My brother in law is a chef. He says "people who claim an onion allergy...just don't like good food."Reason #6722309 why it's okay to hate the muggles.
My wife worked as a chef in a high-end restaurant. She would come home from work and report the most asinine "dietary restrictions" that the patrons reported.
Things like:
"a 30% gluten allergy"
"allergic to raw vegetables; not cooked - but raw"
"allergic to salt"
My all-time favorite was a couple who wanted to split a hamburger; but ordered each half at two different temps (medium, and well).
That's a good case and the kind that's easy for some to miss.I saw my first post-COVID GBS case last night. Strange presentation with lumbar back pain (not that rare in GBS) and proximal > distal leg weakness (turns out after reading some case series, while not classic, also apparently not that rare) with weakness at hip flexors but not as impressive at knees/ankles on exam. Brief mention of some tingling to hands but normal strength there. It really looked like a "can walk but won't walk due to pain and poor copings skills" sort of picture at first. With some grumbling from hospitalist, pt got admitted for can't walk + PT/MRI in AM, found to have COVID on admission screen (no respiratory symptoms or fever, mentioned a mild URI ~ weeks ago) and had elevated inflammatory markers so got tapped and was found to have elevated protein. It's everywhere, watch out and wear your PPE!
So, disappointingly, this one actually might be real - oral allergy syndrome. IgE mediated reaction to a highly conserved protein that denatures with heat. But 100% to the rest of the EDS etc.Reason #6722309 why it's okay to hate the muggles.
My wife worked as a chef in a high-end restaurant. She would come home from work and report the most asinine "dietary restrictions" that the patrons reported.
Things like:
"a 30% gluten allergy"
"allergic to raw vegetables; not cooked - but raw"
"allergic to salt"
My all-time favorite was a couple who wanted to split a hamburger; but ordered each half at two different temps (medium, and well).
Med student here. I personally had a post-viral syndrome that sounds similar to some of what's being described with covid, but mine was after mono. Joint/bone pain, cognitive problems, fatigue, paresthesias in my extremities, and some dysautonomia (though I wasn't a medical person at the time so I didn't know what to call it).
I can say that it was very real (not psychosomatic, thank you very much), it lasted about a year, & I never got back 100% to baseline - just found a new normal. I did not at all benefit from having it, and given that I was in my early 20's at the time and seemingly healthy prior, it felt like it came out of nowhere. I was absolutely terrified that I wouldn't recover and would be functionally disabled. My doctors were all well intentioned (and I saw several), but they had no idea what to tell me other than, "Rest when your body tells you to and try PT. Hopefully it will get better, but we can't promise you anything. Your immune system may be damaged (positive ANA), but we can't find anything else in particular to guide your treatment."
There's still a lot we don't understand about covid, and frankly a lot we still don't know about how the body works. And we'll never learn those those things if we look at patients who have symptoms we can't explain and conclude they must be faking, exaggerating, or that it's really just a psychiatric problem. It does real harm when we choose to ignore part of the data set because it doesn't fit our hypothesis - not to mention the damage it does to individual patients.
There's so many red flags here I don't know where to start. Not even surprised you've seen "multiple different physicians"
You were able to admit that without tapping first?I saw my first post-COVID GBS case last night. Strange presentation with lumbar back pain (not that rare in GBS) and proximal > distal leg weakness (turns out after reading some case series, while not classic, also apparently not that rare) with weakness at hip flexors but not as impressive at knees/ankles on exam. Brief mention of some tingling to hands but normal strength there. It really looked like a "can walk but won't walk due to pain and poor copings skills" sort of picture at first. With some grumbling from hospitalist, pt got admitted for can't walk + PT/MRI in AM, found to have COVID on admission screen (no respiratory symptoms or fever, mentioned a mild URI ~ weeks ago) and had elevated inflammatory markers so got tapped and was found to have elevated protein. It's everywhere, watch out and wear your PPE!
Emergent LP is not indicated for that patient. It’s part of the work up that can be done upstairs.You were able to admit that without tapping first?
Indicated vs required for admission are different.Emergent LP is not indicated for that patient. It’s part of the work up that can be done upstairs.
Indicated vs required for admission are different.
That said if you’re considering GBS don’t you think that warrants a tap as it would change manangement?
Also an incredibly vague presentation. Extreme stretch for GBS imo. No way that gets admitted at my shop, especially right now. You'd need a positive LP for sure. I'd also argue that it would be an "emergent" LP if you're looking for GBS. Guessing a lot more to the story.
I’m not saying this logic is wrong. Just doesn’t seem commonplace.Nonspecific weakness in a young person? Slam dunk admission for neurology consult/MRI in the morning. No need for emergent LP unless fever or other signs of meningitis.
I’m not saying this logic is wrong. Just doesn’t seem commonplace.
“Why can’t they see Neuro in the clinic this week?”
“They’re weak? What if they have GBS?”
“Well do they?”
...
Look fellas. I’ve dealt with dick head academic hospitalist blocking reasonable admissions many a time. In this case I would say an admitting doctor asking for a more specific reason for admission (like what are they going to work up/rule out) or CSF to establish a diagnosis of GBS (which maybe isn’t emergent but usually requires in patient treatment, hence the tap) isn’t unreasonable.Don't be sucked into the mantra that everyone getting admitted to the hospital needs a definitive diagnosis. If you're being wishy-washy and meek with your story and reasoning for admission to the hospital then you're going to get pushback.
Look fellas. I’ve dealt with dick head academic hospitalist blocking reasonable admissions many a time. In this case I would say an admitting doctor asking for a more specific reason for admission (like what are they going to work up/rule out) or CSF to establish a diagnosis of GBS (which maybe isn’t emergent but usually requires in patient treatment, hence the tap) isn’t unreasonable.
They need an emergent/inpatient Neuro consult? Can they see Neuro in the clinic?It's more unreasonable than asking someone to do a non-emergent LP in the ED. Patient needs a Neurology consult with LP done by Neuro/IR. Admit. On to the next patient. The good news is that they can get their inpatient treatment once the results are back from their inpatient LP.
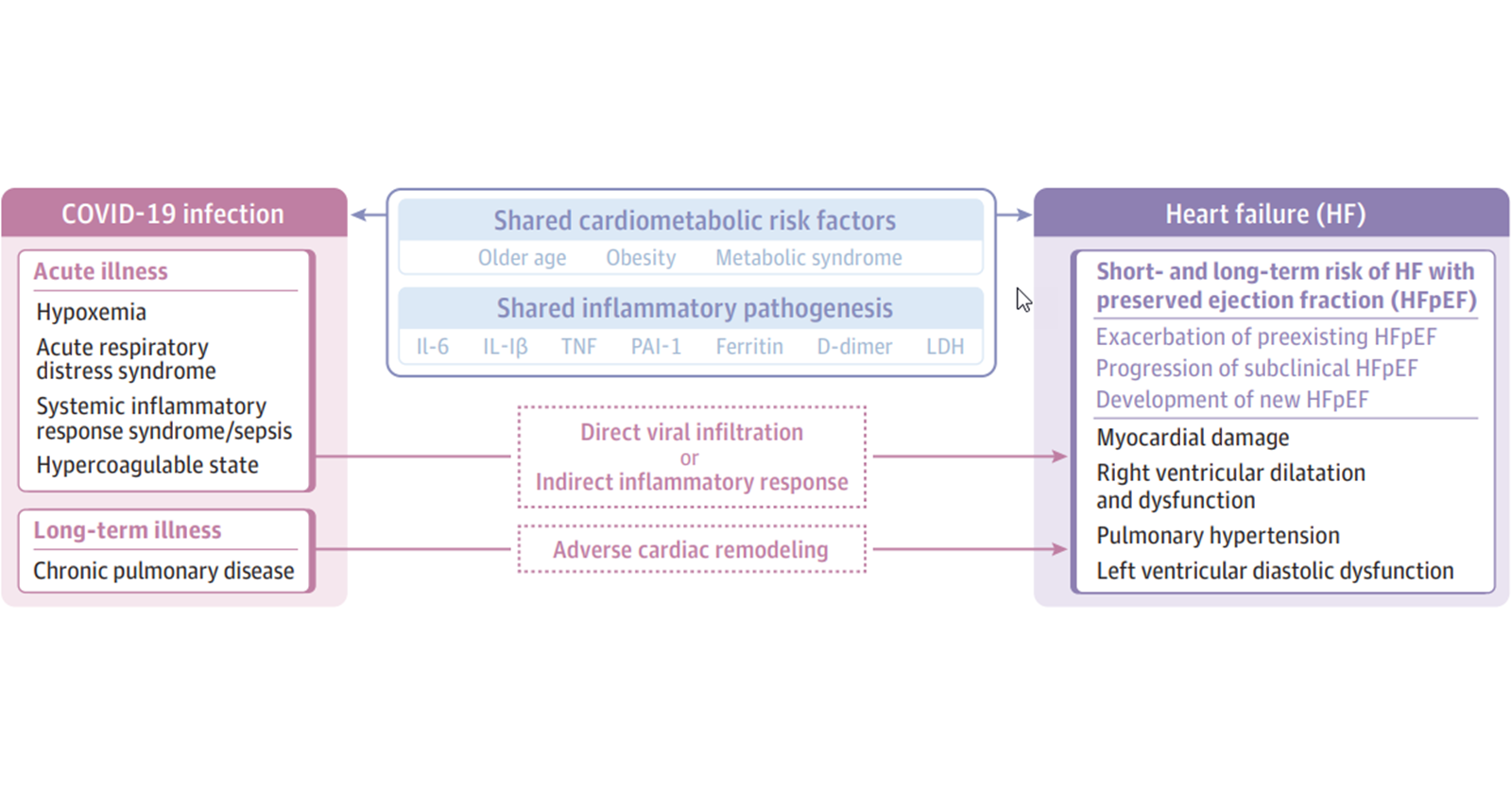
That's a good financial tip. The covid-heart connection is pretty underrated unfortunately90% of heart transplants are due to viral myocardities, usually Coxsackie virus. I would NOT be surprised if the COVID leads to something similar. People here have written about EF decreases after the COVID resolved.
As someone wrote in another forum here on SDN, maybe invest in companies that make LVADs!
The larger the laceration, the larger the scar. I suspect it also holds true that a more severe infection leads to greater myocardial or pulmonary scarring in the form of fibrosis. I doubt most with mild to moderate non-hospitalized infections are going to have significant fibrosis with subsequent reduction in LVEF or PFTs, while those hospitalized or critically ill will end up with worse scars. Most aren’t going to need a transplant or an LVAD. Maybe worth investing though in new medical technology given society’s goals of care.
They need an emergent/inpatient Neuro consult? Can they see Neuro in the clinic?
Not many neurologists can give IVIG in their clinics.They need an emergent/inpatient Neuro consult? Can they see Neuro in the clinic?
Indicated vs required for admission are different.
That said if you’re considering GBS don’t you think that warrants a tap as it would change manangement?
GBS is definitely an emergency....The issue is many times you don’t actually know the true time of onset. When patients finally come in to complain of “few days of weakness” it typically has been a few weeks already of subtle progressive changes (like mild sensory changes, back discomfort) that they may not endorse or notice and impending respiratory failure can ariseI don't actually think GBS is an emergency. It's kind of like COVID - from onset of symptoms to peak physiologic debilitation takes a few weeks. There is really nothing emergent about it unless the patient presents paralyzed and unable to breathe. But you would be thinking of other things at that time anyway and not GBS.
Even though I don't think it's an emergency, it's something that generally should be admitted.
You were able to admit that without tapping first?
Nonspecific weakness in a young person? Slam dunk admission for neurology consult/MRI in the morning. No need for emergent LP unless fever or other signs of meningitis.
If we're talking about true physical exam weakness here then admitting for "MRI in the morning" is inappropriate. I'd argue you need an emergent MRI for neurosurgical intervention. If you have hard neurologic signs then you're at the point of "time is brain" or neuropathways in this case. Other spinal cord pathologies exist beyond cauda equina (which presents classically less than 50% of the time). If negative then do the LP since this isn't classic GBS presentation. Then admit.
Most "admission MRIs" get de prioritized to nonstat. He might get it two days from now. Now he can't walk. Pretty much a slam dunk malpractice case for nsg to throw EM under the bus.
They need an emergent/inpatient Neuro consult? Can they see Neuro in the clinic?
GBS is definitely an emergency....The issue is many times you don’t actually know the true time of onset. When patients finally come in to complain of “few days of weakness” it typically has been a few weeks already of subtle progressive changes (like mild sensory changes, back discomfort) that they may not endorse or notice and impending respiratory failure can arise
It’s not like they sit around at home checking deep tendon reflexes daily
Not where I trained...I looked at the procedural requirements in the Internal Medicine RRC and it didn't have LP. Internal medicine's procedural requirements are becoming fewer and fewer as decades go byInternists are also credentialed to do lps (lol not gonna happen) and they have multiple consulting services that can do them as well (what will happen, usually rads or ir).
Not where I trained...I looked at the procedural requirements in the Internal Medicine RRC and it didn't have LP. Internal medicine's procedural requirements are becoming fewer and fewer as decades go by
I've never seen any internist do a procedure. They cant/won't do even a simple lac repair or place a rhino rocket on a floor patient. They call me all the time for this BS and I politely refuse.
I saw an internist do a procedure once. He popped a zit on himself in the hospital bathroom after the Derm 2nd year refused to do it.Yup they don't do s^it. I'm not even sure they touch patients during a physical exam.
Not where I trained...I looked at the procedural requirements in the Internal Medicine RRC and it didn't have LP. Internal medicine's procedural requirements are becoming fewer and fewer as decades go by
I would let a 2nd year female derm resident pop a zit on me.I saw an internist do a procedure once. He popped a zit on himself in the hospital bathroom after the Derm 2nd year refused to do it.
