- Joined
- May 7, 2014
- Messages
- 1,657
- Reaction score
- 3,473
Discuss
 jamanetwork.com
jamanetwork.com
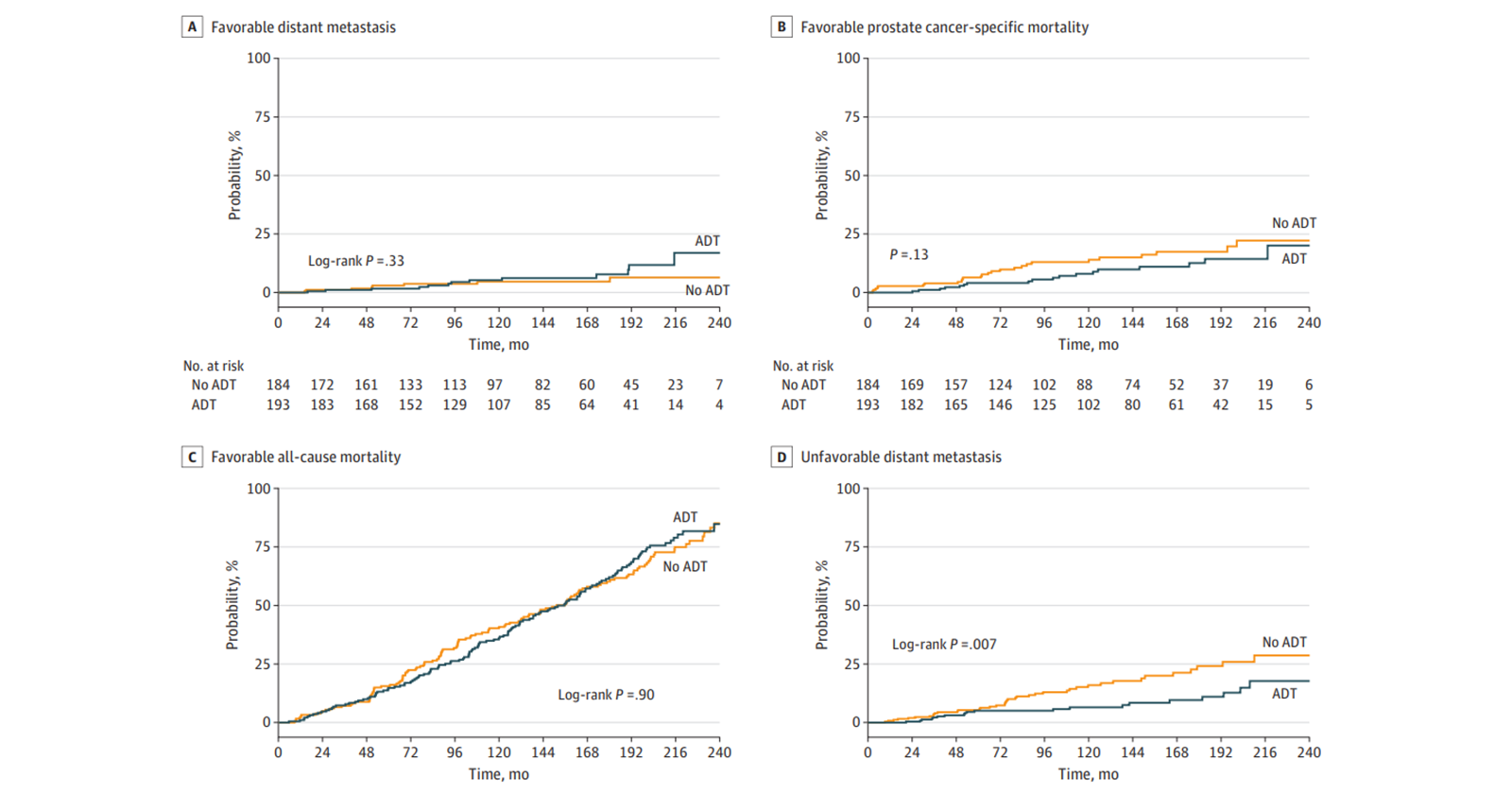
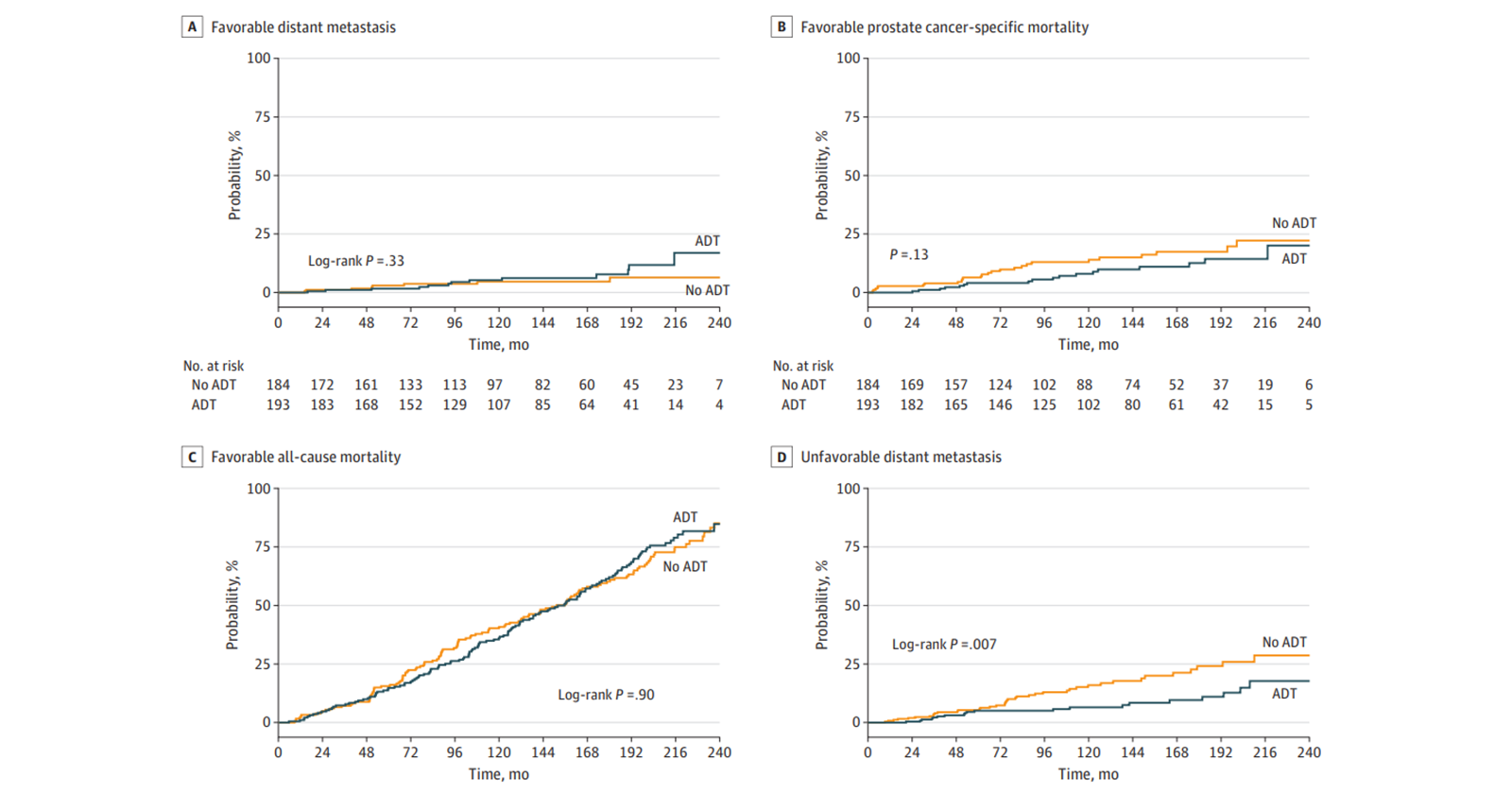
Effect of ADT on Long-term Outcomes of Favorable or Unfavorable Intermediate-Risk Prostate Cancer
This secondary analysis of a randomized clinical trial examines the effect of androgen deprivation therapy (ADT) during radiotherapy in patients who were classified as having either favorable intermediate-risk or unfavorable intermediate-risk prostate cancer.
Last edited by a moderator:
