- Joined
- Feb 9, 2006
- Messages
- 557
- Reaction score
- 51
Any opinions on people's favorite dose of duramorph to use with bupivacaine for SAB for c-sections?
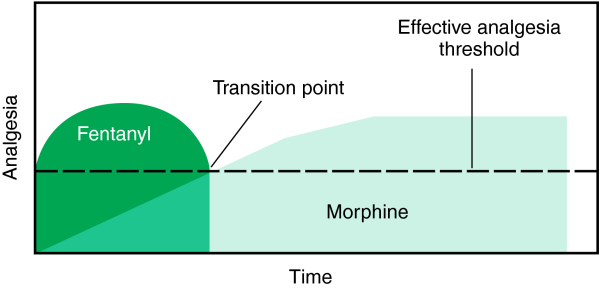
Honestly, during residency, we mainly used fentanyl for our CSXN spinals, but the new practice I'm with uses duramorph for about every section. Opinions on adequate doses (0.2-0.4mg duramorph?) Vs side effects (Itching, resp depression)?
Opinions welcome....any good recipes are always appreciated!!
Honestly, during residency, we mainly used fentanyl for our CSXN spinals, but the new practice I'm with uses duramorph for about every section. Opinions on adequate doses (0.2-0.4mg duramorph?) Vs side effects (Itching, resp depression)?
Opinions welcome....any good recipes are always appreciated!!