What’s your guys’ approach for the patient who gains only 50% improvement following C3-5 RFA? Can you start the whole process over targeting the adjacent levels?
I think we pain physicians typically target C3-5 even though C2-3 and C5-6 are the most common levels implicated in facetogenic neck pain.
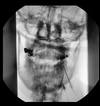
look at imaging again and also do another patient history/exam.
First question is do they have significant upper neck pain and/or headaches? if yes, then consider C2-C3 though most of us will capture TON while lesioning C3. However, be sure to directly palpate C2-C3.
Second question is do they have significant neck pain inferior to your lesion location (C5-C6 or C6-C7)? Be sure to directly palpate C5-C6, C6-C7
Third question- "is the remaining 50% of their pain in the middle 80% of their neck( C3-C5 area). If so, they got 50% relief either because half of their pain is from DDD or because you didn't do a thorough lesion C3-C5.
Assuming good technique, the most common issue is they would benefit from C6 RFA. When this happens I tell the patient that in 6 months, we can add C6 if they pay for that add on level in cash, or if they want we can repeat the MBB, targeting C4-C6, and then just do C4-C6 RFA going forward.
If a patient doesn't have significant headaches and never had ACDF, I will rarely include C3.
C4-C6 RFA is more useful for more patients with non surgerized necks compared with C3-C5 RFA, (unless the C3-C4 looks particularly bad on imaging or you strongly suspect cervicogenic headaches). I rarely do C3-C5 RFA unless they had C5-C7 ACDF.
C4-C6 provides better relief for most patients without cervicogenic headache and without prior ACDF.