- Joined
- Nov 28, 2014
- Messages
- 4,212
- Reaction score
- 15,007
Like I get when it’s indicated and understand the side effects. But is there any reason not to just take one to take one?
Because 10 year risk is what we have to work with. That and our own judgement when called for.Fantastic post above. I would also add maybe checking an Lp(a) once. Keto in specific ive read may lead to advanced glycation end products, which maybe be bad…?
I do feel ascvd is a little short sighted. Why would i wait for someones 10 year risk to be 10%? I would think it’s better to treat someone who’s 20 year risk is 10%. Or why not 30 year risk…
Fantastic post above. I would also add maybe checking an Lp(a) once. Keto in specific ive read may lead to advanced glycation end products, which maybe be bad…?
I do feel ascvd is a little short sighted. Why would i wait for someones 10 year risk to be 10%? I would think it’s better to treat someone who’s 20 year risk is 10%. Or why not 30 year risk…
While I fully agree with your statement, I must highlight that not enough effort is done for the "dietary and lifestyle change."Yeah we don’t do a calculator about smoking in ten years and if they have a low risk for lung cancer by smoking less than half a pack a day we don’t intervene.
Similar to how the data with blood pressure that the closer to 120/80 the better. If you have high lipids, and they remain high despite dietary and lifestyle change. You should be on a statin. Atherosclerosis and cardiovascular disease is the number one killer.
@NewYorkDoctors Am I correct in saying you would disagree with this? For someone who is active, eats healthy, and is lean high lipids (specifically LDL) is NOT an indication that they should be on a statin?Yeah we don’t do a calculator about smoking in ten years and if they have a low risk for lung cancer by smoking less than half a pack a day we don’t intervene.
Similar to how the data with blood pressure that the closer to 120/80 the better. If you have high lipids, and they remain high despite dietary and lifestyle change. You should be on a statin. Atherosclerosis and cardiovascular disease is the number one killer.

Yeah, but those dudes are perseverating on about 200 other ridiculous things as well, so take that with a grain of salt.@NewYorkDoctors thanks for the reply. I ask because I have friends within my natural bodybuilding circle who perseverate on their "not ideal" LDL numbers thinking they definitely need to be on a statin. These are guys who are relatively lean, active, and eat a healthy diet.
Statins also aren't great for connective tissue/tendon health.
Since those individuals are into the health lay media , refer them to that “doctor” on twitter who is jacked (probably on TRT) and did a ctca and cac on himself and was totally clean@NewYorkDoctors thanks for the reply. I ask because I have friends within my natural bodybuilding circle who perseverate on their "not ideal" LDL numbers thinking they definitely need to be on a statin. These are guys who are relatively lean, active, and eat a healthy diet.
Statins also aren't great for connective tissue/tendon health.
Then they'll get swindled into a bunch of other questionable tests, supplements, and "therapies" 😂Since those individuals are into the health lay media , refer them to that “doctor” on twitter who is jacked (probably on TRT) and did a ctca and cac on himself and was totally clean
It’s funny how you say you dont go out of your way to promote a keto diet, but you have had numerous posts where you kinda do…it’s not a diet that is necessarily safe or healthy and for most, not sustainable in the long run…im no lipid expert. so no one should quote me on anything.
but just having high LDL alone in the setting for primary prevention should invite some degree of introspection on the case rather than a reflex maximum statin time
Yes I know the ACC/AHA guidelines state:
4. In patients 20 to 75 years of age with an LDL-C level of 190 mg/dL (≥4.9 mmol/L) or higher, maximally tolerated statin therapy is recommended.S4.3-2,S4.3-20–S4.3-25 Included from recommendations in the 2018 Cholesterol Clinical Practice Guidelines.S4.3-1
Moreover, the UTD authors state:
LDL-C greater than or equal to 190 mg/dL — For all patients with LDL-C ≥190 mg/dL (≥4.9 mmol/L), we do a work-up for familial hypercholesterolemia (FH), and if present, treat accordingly. The work-up and management of FH are discussed separately. (See "Familial hypercholesterolemia in adults: Overview" and "Familial hypercholesterolemia in adults: Treatment".)
If the patient does not have FH, we treat them with a high-dose statin therapy. As an example, we may start these patients on atorvastatin 40 mg daily or rosuvastatin 20 mg daily. The dose and intensity of different statin medications are described in detail separately.
A CVD risk calculation may be unnecessary for individuals with an LDL-C ≥190 mg/dL (≥4.9 mmol/L), because we usually prescribe statin therapy for them based on the elevated LDL-C level alone.
It is interesting how these recommendations do NOT provide citations
A quick review of the Pubmed shows:
Low-Density Lipoprotein Cholesterol Lowering for the Primary Prevention of Cardiovascular Disease Among Men With Primary Elevations of Low-Density Lipoprotein Cholesterol Levels of 190 mg/dL or Above
Analyses From the WOSCOPS (West of Scotland Coronary Prevention Study) 5-Year Randomized Trial and 20-Year Observational Follow-Up
Results
Among 5529 individuals without vascular disease, pravastatin reduced the risk of coronary heart disease by 27% (P=0.002) and major adverse cardiovascular events by 25% (P=0.004) consistently among those with and without LDL-C ≥190 mg/dL (P-interaction >0.9). Among individuals with LDL-C ≥190 mg/dL, pravastatin reduced the risk of coronary heart disease by 27% (P=0.033) and major adverse cardiovascular events by 25% (P=0.037) during the initial trial phase and the risk of coronary heart disease death, cardiovascular death, and all-cause mortality by 28% (P=0.020), 25% (P=0.009), and 18% (P=0.004), respectively, over a total of 20 years of follow-up.
Conclusions:
The present analyses provide robust novel evidence for the short- and long-term benefits of lowering LDL-C for the primary prevention of cardiovascular disease among individuals with primary elevations of LDL-C ≥190 mg/dL.
Okay if you just read the abstract and decided to call it a day because you're a busy doctor who can't be bothered to read the whole thing because... EMRs are hard....
You would have missed the the fact that many of the enrolled patients are not quite "healthy."
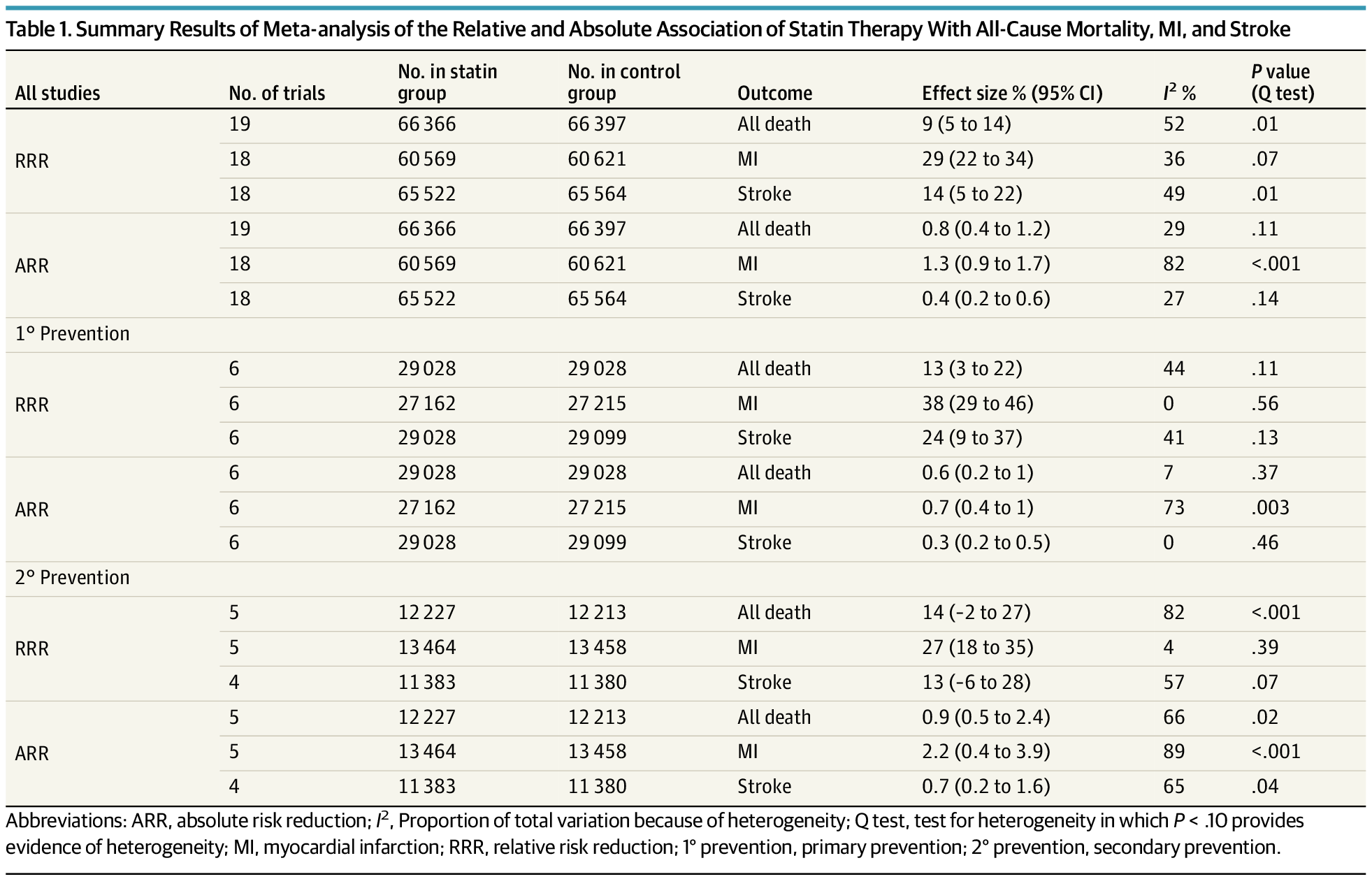
View attachment 369919
look at the baseline lipids. those are the classic dyslipidemic patients with high totla, high LDL, low HDL, and high triglycerides. plus their BP was already in the 2017 AHA class 1 hypertension range and half of the smoked!
You will get zero arguemtns from me that these kind of "unhealthy metabolic syndrome patients" should be on statins for primary prevention if their ASCVD, Reynold's, or Framingham risk score is high.
There is very little high quality data on the ketogenic diet lipid profile. Most pro keto physicians state that (on a case by case basis) these patients have low hsCRP, low small desnity LDL particles, no evidence of subclinical ASCVD when doing things like CAC, CTCA, CAS U/S, aorta U/S, etc.....
Granted, this they will never fund this kind of research because eating healthy will ultimately ruin the bottom line of Big Food and Big pharma, but I digress.
but if we just use the good old fashioned AHAACC ASCVD risk score calculator for... a 40 year old.. who went full keto (and also made sure not to go sodium overload) who is normotensive 110/70, no DM, no smoking whose profile is let say... Total Chol 350 HDL 90 TG 50 LDL (calculated) 250 (i'm going to include all the possibilities of sex and race)
ASCVD (Atherosclerotic Cardiovascular Disease) 2013 Risk Calculator from AHA/ACC
The 2013 ASCVD Risk Calculator is a vital tool for estimating the 10-year risk of heart disease or stroke. Developed by the American College of Cardiology (ACC) and the American Heart Association (AHA), this calculator helps healthcare providers assess cardiovascular risk and guide management...www.mdcalc.com
Male - White - 1.1% 10 year
Male - AA -2.3%
Male - Other - 1.1%
Female - White 0.5%
Female - AA - 0.1%
Female - Other - 0.5%
Let's do 65 year old now
Male - White - 10.4%(can have discussion about changing the keto diet first rather than using statins)
Male - AA - 7.5% (can have discussion about changing the keto diet first rather than using statins)
Male - Other - 10.4% (can have discussion about changing the keto diet first rather than using statins)
Female - White - 4.6%
Female - AA - 8.3% (can have discussion about changing the keto diet first rather than using statins)
Female - Other - 4.6%
bottom line - dont look at LDL > 190 and automatically reflex to statins. I admit most patients are "unhealthy less fit metabolic syndrome" and at the end of the day we will start them anyway.... but we are doctors! Not NPs/PAs who follow an algorithm only.
Again I don't go out of my way to promote the keto diet. most patients mess it up due to not cutting the carbs down enoguh and just eating too much unhealthy fats and salt ("dirty keto").
It’s funny how you don’t bother to read my prior post in this thread stating I don’t promote it but if a patient is on it then what am I going to say to this patient ?It’s funny how you say you dont go out of your way to promote a keto diet, but you have had numerous posts where you kinda do…it’s not a diet that is necessarily safe or healthy and for most, not sustainable in the long run…
I wouldn't know what I am talking about lol. I am just talking about this topic as an Internist and someone interested in this topic.If I DM any of you intelligent IM docs my Cardio IQ data, will you tell me what to do with it? Not in a "medical advice" way, but in a "friends having a casual conversation" way?
