- Joined
- Dec 17, 2007
- Messages
- 3,796
- Reaction score
- 5,427
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
I thought, I'd start an ASCO 2025 thread.
Interesting abstracts
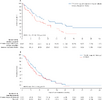
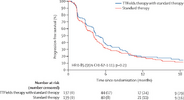
1. Concurrent and adjuvant Pembrolizumab in primary radiochemotherapy for SCCHN
2. Adjuvant Nivolumab after postoperative radiochemotherapy for SCCHN
3. MWA or SBRT for liver metastases
4. Low-dose olanzapine for nausea
A few breast RT-omission trials are apparently in progress

Interesting abstracts
1. Concurrent and adjuvant Pembrolizumab in primary radiochemotherapy for SCCHN
2. Adjuvant Nivolumab after postoperative radiochemotherapy for SCCHN
3. MWA or SBRT for liver metastases
4. Low-dose olanzapine for nausea
A few breast RT-omission trials are apparently in progress