Scarb, is there literally anything that you do that falls in line with what is generally accepted as normal practice? I have the sense that you just like to debate, but you seem to almost always take a contrarian view. You don't treat nodes, you don't boost...
View attachment 272111
FWIW Whelan has said himself that he typically boosts, despite the lack of a mandated boost on his trial.
Boost!
Well heck it's the Internet... and SDN... and I'm a misanthrope. A perfect debate stew.
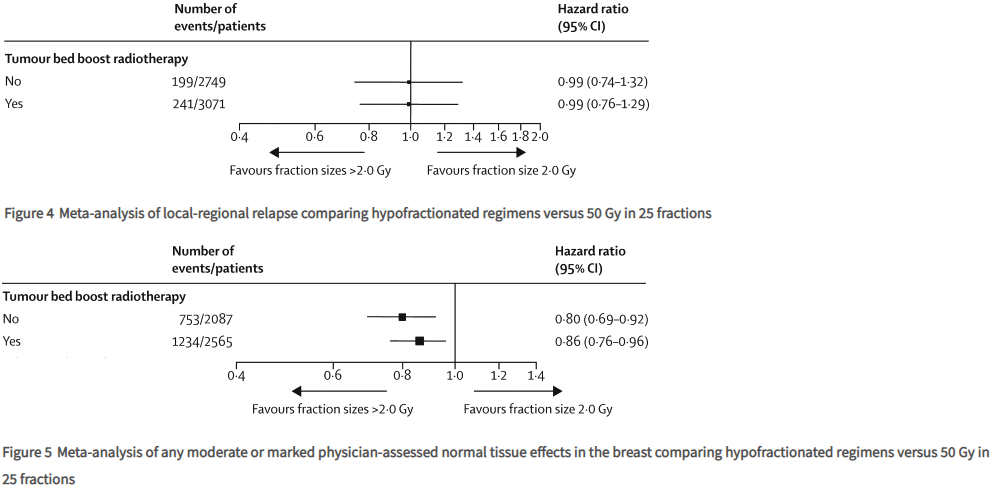
I have seen in my own neck of the woods the local academic center give breast boost to ALL hypofx patients. So which: "blindly" apply to all, or choose judiciously? Upon whom is breast boost in hypofx shown to influence outcome?
If someone ran a trial that established a new standard and publicly announced he "typically" never treats in the manner of the trial, that would "typically" be a news item. AFAIK boosting in hypofx is not "normal practice," nor is routine RNI (especially for N0 patients, of which ~50% made up the
EORTC RNI trial e.g., and they kind of derived the biggest benefit from RNI vs N+).
I have posted this before but over the last decade only
~4 out of 100 rad oncs worldwide routinely applied RNI to all 3 sites of IMN/sclav/axilla when doing RNI. Yet
MA.20--a trial where all 3 RNI sites were treated in ~100% of patients on the RNI arm--is ostensibly the reason RNI is "normal practice" as you say? What use are these Canadian trials if they establish new practices but then no one treats according to the trials, not even the guy who ran the trials*? What
is normal? BTW, I never said I don't treat (any) nodes. However, yes, I never boost w/ hypofx. (Non-boosters should be sitting pretty when APM comes down the pike...
it's predicted we'll all be treating breast in 5 fractions one day anyways rendering all this brouhaha moot.)
Why say this is "normal practice" (or "I usually look for reasons not to boost but this one ain't it, chief") when there's
weak to
no data? Or
conflicting data in opposite directions. I'm just a real skeptic when people think they have the market cornered on the "right" answer when the data is a big mishmash of low single digit numbers positive and negative sans any effect on natural histories. But yet, this actually describes much of "normal practice" in radiation oncology.
*What Whelan once said about the boost:
In our trial, additional boost radiation to the lumpectomy site was not used, because data from randomized trials supporting its efficacy were not available. Since the completion of this study, results from randomized trials indicate that boost radiation has a modest impact on local recurrence at the expense of cosmetic outcome. In the recently published EORTC trial, the rates of local recurrence at 5 years were 7.3% in the arm receiving breast irradiation alone and 4.3% in the arm receiving the boost radiation. The observed local recurrence rates in our trial were lower: 3.2% in the long arm and 2.8% in the short arm. Although there are limitations to cross-study comparisons, there are some important differences between the two studies. The EORTC trial was conducted in women with negative (78%), positive (21%), or unknown (1%) axillary lymph node status, whereas we enrolled only women with a negative axillary lymph node status. In the EORTC trial, 28% of women received adjuvant systemic therapy, whereas in our trial 52% of women received systemic therapy. In the EORTC study, the benefit of boost radiation appeared mainly in women 50 years of age or younger; in these women, the rate of local recurrence was high—as high as 20% in women who were aged younger than 40 years. In our trial, no difference was detected between groups including younger women; in younger women, the rates of local recurrence were low, especially for women treated with the shorter course of radiation therapy (i.e., 3.6%). For such women, we would postulate that the benefit achieved with boost radiation would be of a relatively small magnitude. Although Bartelink et al. recommend boost treatment for all women who are younger than 50 years old, in our view, this remains an area for future study.