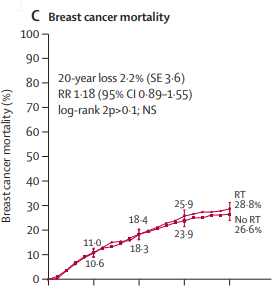
41 y/o female, 6cm IDC, 2 enlarged axillary lymph nodes on preop imaging (2cm and 1.5cm respectively), IDC, ER 10%, PR/HER-2-negative. 2cm axillary node core biopsy negative (clip placed at time of biopsy). BRCA-negative. Received neoadjuvant ACT with imaging showing complete resolution of breast mass and "normalization" of both enlarged nodes. (Per imaging, the 1.5 cm node initially showed thickened cortex but now normalized with fatty hilum). Got simple mastectomy + SLNB + immediate implant reconstruction. 0/1 nodes + (previously clipped node). Path CR. Surgeon supposedly presented at her "local tumor board" where rec was for No RT.
Would you radiate?
Would you radiate?
Last edited: