Good points from everyone. All were brought up by our department. As stated earlier the decision was to proceed with a palliative Girdlestone procedure after all other parties decided surgical intervention was the only viable definitive analgesic option.
Partial alpha blockade was pursued pre-op with 48 hours of prazosin.
Fascia iliaca catheter loaded with a relatively high concentration/volume of Ropivacaine immediately prior to transfer from the ward - then removed to not get in way of surgery.
THRIVE (Transnasal Humidified Rapid-Insufflation Ventilatory Exchange) + facemask --> SpO2 100%

Awake art. line.
Baby boluses of ketamine --> rolled fracture side down.
Homoeopathic vasopressin infusion commenced.
Intrathecal catheter inserted.
Micro-doses of Heavy Bupivacaine 0.5%
Total dose = 2mL over 30 minutes.
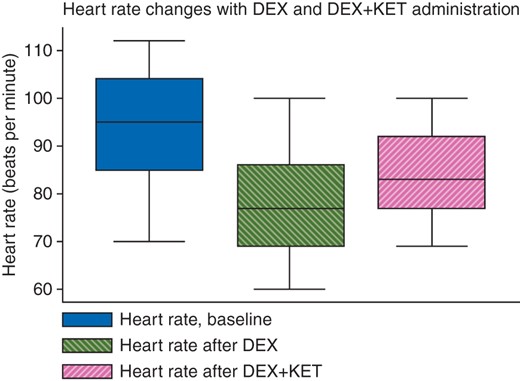
Traintrack vitals (200/105 since entering operating theatre).
Rolled onto back --> momentary HD instability --> straight leg raise --> improvement --> 200mL fluid bolus --> rallied.
Shifted to operating table + rolled fracture side up --> momentary HD instability --> vassopressin increased slightly --> rallied.
Senior surgeon present.
Skin to skin time = 15 minutes. Total blood loss = ~50mL.
Moved to recovery.
Vasopressin ceased.
Femoral nerve catheter re-inserted.
THRIVE ceased --> SpO2 immediately 50% despite 15L non-rebreather --> THRIVE re-initiated.
SpO2 ~85% on THRIVE overnight.
Downtitrated next morning.
Post-op pain controlled with femoral nerve catheter and low dose PRN opioids + simple analgesia.
At baseline 24 hours later: SpO2 80% on 8L.
Discharged home with pain improving and catheter removed.
Discussion:
Although everything went exactly as planned and the patient got an excellent result; this was unexpected. The outcome did nothing to sway the divided opinions within our department or other departments. In the end the patient received a purely palliative procedure and everything went right for them. Had they passed on would this have been appropriate? I doubt anybody's mind would have been changed regardless of the outcome.
What is key to note is this is what the patient and family wanted; this is what was offered by orthopaedic surgeons; and they will most likely go on to live a few more months in relative comfort in the place they wish to be. Palliation should focus on comfort, respect and autonomy. For that reason I am in the "exclude all other analgesic modalities and then proceed with definitive palliative surgery" camp. I'm sure many disagree.