Old thread but important thread...
- The paper that
@Neuronix posted above is from C. Perez (Washington Univ) during RT alone era (no concurrent chemo) and LDR.
Pezer recommended overall Tx time
< 49 days (7 weeks).
- The latest ABS compendium for brachytherapy was last updated in 2019:
Compendium of fractionation choices for gynecologic HDR brachytherapydAn American Brachytherapy Society Task Group Report
On page 3, excerpts:
"...Point A-based prescription. Treatment with EBRT (with or without concomitant chemotherapy) and brachytherapy should be completed in less than 7-8 weeks as better local tumor control and survival can be expected (11,12). Some institutions interdigitate HDR brachytherapy with EBRT to shorten the total treatment duration, but this can only be carried out if adequate dose can be given to the residual disease. The most recent ABS consensus guidelines for HDR definitive brachytherapy for cervix cancer are from 2012 (8)..."
- So for 2022, when the vast majority of pts receive concurrent chemo, I am OK with overall Tx time of 49 days to 56 days. Basically, let's say the EBRT is 45 Gy and completed in 5 weeks (assuming no interruption), then you have 2-3 weeks to do the HDR implants. If you do 2 HDR procedures/week, and assuming you do 3-5 fractions (max = 5 HDR appliactions) then you should be fine.
- On the comment above re
3 fractions.
It was first pioneered by McGill, the first ever article on HDR for cervix (they started this HDR program in 1984, way before any centers in Canada or USA) to publish in RedJ circa (RT alone bc data for concurrent chemo came later in the late 1990s). If you take this set of data from McGill, add about 10-12% to the survival figures and you should get modern outcome data...
* Data from 1984-1989 (n= 187 during 5 yr-period, high-volume center!)
* McGill data updated in 2005 in Gyn Onc; data from 1984 and 1997, n = 282:
To evaluate the long-term treatment outcome of patients with carcinoma of the cervix treated with high dose rate brachytherapy (HDRB) using a small nu…

www.sciencedirect.com
Kind of funny ABS comments saying "resource-poor countries" comment...
- Anyway, for 2022, I am OK with
8 Gy x 3,
7 Gy x 4, or
6 Gy x 5.
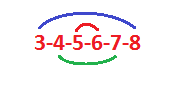
If one is too old to remember anything, a memory aid is
3-4-5-6-7-8...lol.
- I have done 8 Gy x 3 for over 15-20 yrs, it works very well.