- Joined
- Nov 21, 1998
- Messages
- 12,566
- Reaction score
- 6,959
Anyone have any experience with this? The buzz from ASPN is positive...

I think a lot of the buz may be coming from a speaker who has significant ownership in the company or so I have been told.
Not hard to get positive provocative maneuvers when everything hurts.I saw a 32 yo F last week with an SIJ fusion done in her late 20s. I'm 99% sure she got a fusion for fibromyalgia.
I saw a 32 yo F last week with an SIJ fusion done in her late 20s. I'm 99% sure she got a fusion for fibromyalgia.
Well I presume the bs si fusion gives the right diagnosis for the scs..... genius!Just wait. Within a few years she will have an SCS and Vertiflex Superion
These marketed to pain docs are just little wedges of allograft.
Is there office reimbursement?
sij fusion defies logic, but then again so does lone commie
On the other hand, with your experience you seem well positioned to earn yourself a nice little golden parachute - just pick one of those old techniques, do a small RCT showing efficacy, and sell it as the next miracle cure for axial low back pain. IDET’s probably due for its next 15 minutes of fame, right?I agree-
These guys forget that SI joint fusions were all the rage in the early 90s- it ended in disaster. What happened was that all these people beat the hell out of their hip joints through this very weird "gangsta rappa" gait disturbance in a few years after the fusion. It was abandoned. Those patients all got hip arthroplasties, so the orthopods were happy. Oddly, they still had that peculiar gait, and you could spot them walking down the hall of the clinic.
Then SI fusions became popular again in about 2006-2008 with similar outcomes. The contention then was that the hardware was just not up to snuff ten years prior, so it deserved another try. When chatting with some of the new neurosurgeons, I told them to ask their senior partners about their experience before embarking on doing such cases.
Now I am glad to see that it has been resurrected for another try, as it is like a "zombie" procedure that just won't die. Perhaps it needs to be shot in the head, as this appears to be the only method that kills zombies (I personally have no experience in zombie killing).
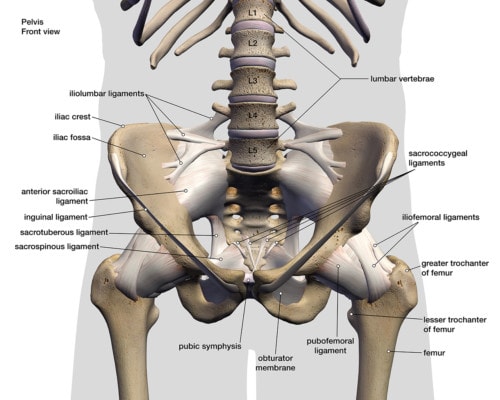
How, exactly, does one determine that an SI joint is "unstable"? I understand the concept very well with a spondylolisthesis, but I am not aware of dynamic studies that demonstrate SI joint "instability" and thus pain. Further, these forces (when one is fused) have to go somewhere. Where does the force go if the gliding joint is fused? Laterally to the hips- it is just plain physics folks. Now if one has pain at rest over the SI joint (with no motion), how can one think that the joint needs to be fused???
SI joint pain most likely exists; however, I would offer the majority is sclerotomal referred pain and is "diagnosed" simply by tenderness over the SI joint (Fortin's finger test) and response to a diagnostic injection, which can have its own problems. We all do IS joint injections and they seem to work on some patients. I have done SI rf (I am really not sure about that one); both of those are reversible and do not result in appreciable harm to the patient. I can't wait until someone (and it will happen) kills someone by getting a little aggressive and tears into the iliac vessels. It's always funny until someone loses an eye! Ever see one of those with a lumbar disc? It ain't pretty.
Let's see................................ Racz catheter, IDET, decompressor, nucleoplasty, pulsed rf, MILD, X-Stop, intradiscal rf, prolotherapy....................................
another body on the rubble heap of procedures that were once all the rage. This is the problem with pain management- implementation of procedures well before any significant data showing efficacy. There is always someone out to make a buck with these, at the expense of our patients. Let's try to be a little more skeptical and demand some degree of evidence before embracing such treatments.
On the other hand, with your experience you seem well positioned to earn yourself a nice little golden parachute - just pick one of those old techniques, do a small RCT showing efficacy, and sell it as the next miracle cure for axial low back pain. IDET’s probably due for its next 15 minutes of fame, right?
All of us have been sucked into performing these garbage procedures only to find out that they don’t work. In 2019 this is an even bigger problem because of social media. The reps and their companies know how to stoke the egos of young docs and get them to do hundreds of these procedures so they can post a selfie on Facebook.
except I am unwilling to even take a Tylenol for myself. there are a lot of other people who deserve a Tylenol more than me....Yep- And we all have been fooled in the past. I am a pretty gullible guy and can be talked into most anything, but I think I am getting better.
There is the fear of become outdated and passe, vs being conservative and embracing only treatments with strong evidence. It is a balancing act we all face.
I think the best course is to look at something and ask yourself if you would do it on YOU, if you were in the patient's shoes. It is weird, but that is a good metric.
except I am unwilling to even take a Tylenol for myself. there are a lot of other people who deserve a Tylenol more than me....
except I am unwilling to even take a Tylenol for myself. there are a lot of other people who deserve a Tylenol more than me....
Pretty simple procedure. Just little cubes of allograft. Training was quick and simple.
1. Limited data obviously.
2. Misplace the device and bag sacral nerve root. Fracture the pelvis or sacrum potentially? They said no major complications in 400 cases.
3. No
4. The allograft should incorporate and not be possible to remove.
I have no disclosures with these companies:
For the postlaminectomy patient that responds to the SIJ injection x 2 - it has excellent results. Great option because SIJ rfa doesnt reimburse or is considered investigational.
Spine Surgeons wont operate or utilize SI bone on the medicare population. Some commercial insurances cover minimally invasive approach but that patient doesnt present all too often. Once lumbar fusions become less prevalant so will SI fusions. For now these are the options. A lot of the “veteran” pain docs also created the opioid epidemic and had no problem getting lunches, speaking at dinners for opioid companies - and now that these non-opioid therapies are coming out will exhaust energy trying to trash them - maybe should have taken that stance with opioids and we wouldnt be here
The opioid epidemic does not justify embracing dubious procedures. I did take a stand on opioids- no one wanted to listen to me and simply made disparaging remarks about me being a worried grandmother. Oddly, the very same people who fueled the opioid epidemic just put on a new hat and are suboxone advocates today and claimed they knew opioids were "bad" all the while!
Again- this procedure and concept never worked in the past. I fully support any new treatments that are effective. However, I have lived through this aspect of delving into any new procedure that comes along, only to have my head handed to me more times than I can count.
1. How do you diagnose SI joint instability?
2. Most "SI joint pain" is referred and not from the joint itself
3. Why didn't the SI joint fusions work in the past?
4. Why do you think that fusing an SI joint will not cause arthritis in the hip, as it did in the past? Just as the lumbar fusion that presumably created SI joint pain, you are just transferring forces to the hip joints.
5. Would you have this done on yourself?
6. If you do a discogram on levels above a fusion (I know- not done anymore), why does the patient hurt over the SI joint?
Before exposing patients to such procedures, why not study them in detail before they are rolled out for "prime time"? I am all for new technology, but pain management is notorious for rushing forward with unproven treatments, only to find out later they don't work.
Bob- it sounds like you are a bright, energetic guy who is looking for new treatments for your patients. That is great! We won't advance at all as a specialty unless someone is pushing the envelope. Just be careful and don't risk your credibility by instituting too many new treatments without a good track record. I don't want to sound like a "negative Nancy" all the time, but I have just been burned too many times with new procedures that didn't work out.
See attached.
Did they really try to get you to put a monthly number on CornerLoc? I don’t see it being a routine procedure for most pain physicians.Interesting perspective. Thanks for posting. At least now I will have something to talk about with patients who have SIJ pain and fail the standard therapies. I couldn’t promise CornerLoc their desired minimum of X number of cases per month so I guess I will never get trained or be a CornerLoc Center of Excellence.
why marries? surgeons fuse the SI joint and fuse the back and discharge the patient for their clinic in 6 weeksSorry, but I feel it is downright terrible for a pain doc to fuse the SIJ, as we truly know better.
Evidence is terrible, and you’ve maimed them for life afterwards.
Did they really try to get you to put a monthly number on CornerLoc? I don’t see it being a routine procedure for most pain physicians.
My recollection was 2-3/month. I think I might be able to get 2-3/year tops unless I change my treatment paradigm to everyone who gets relief from 1 SIJ injection gets an SIJ fusion when the pain returns. That of course would need to be followed by Vertiflex, Intracept , DCS and then cluneal nerve PNS. That is of course if any of those procedures are available to me as a Tin Level provider unable to award loyalty points to the patient.What was the number per month or year for their ‘requirement ‘?
Agree, it is a 10 case/year type procedure. We have a distributor here. It could be your distributor not the company that is the issue.
My recollection was 2-3/month. I think I might be able to get 2-3/year tops unless I change my treatment paradigm to everyone who gets relief from 1 SIJ injection gets an SIJ fusion when the pain returns. That of course would need to be followed by Vertiflex, Intracept , DCS and then cluneal nerve PNS. That is of course if any of those procedures are available to me as a Tin Level provider unable to award loyalty points to the patient.
It is a lot cheaper than that. That is the open si fusion code they are looking at.
This is an honor only bestowed on the TOP PROVIDERS who sell, I mean implant, at least 10 per month. Additional incentives available for bilateral procedures...How can I too become a Tin Level provider? I have been stuck on paper mache level for some time.
This is an honor only bestowed on the TOP PROVIDERS who sell, I mean implant, at least 10 per month. Additional incentives available for bilateral procedures...
