- Joined
- Nov 13, 2013
- Messages
- 3,222
- Reaction score
- 4,537
"The case started with a dental assistant who went into surgery for carpal-tunnel syndrome and ended up with a perforated esophagus...
Kalitan filed the malpractice case in 2008 in Broward County and named a series of defendants, including the North Broward Hospital District, an anesthesiologist, a certified registered nurse anesthetist and a company that contracted to provide anesthesiologists and staff to the hospital district.
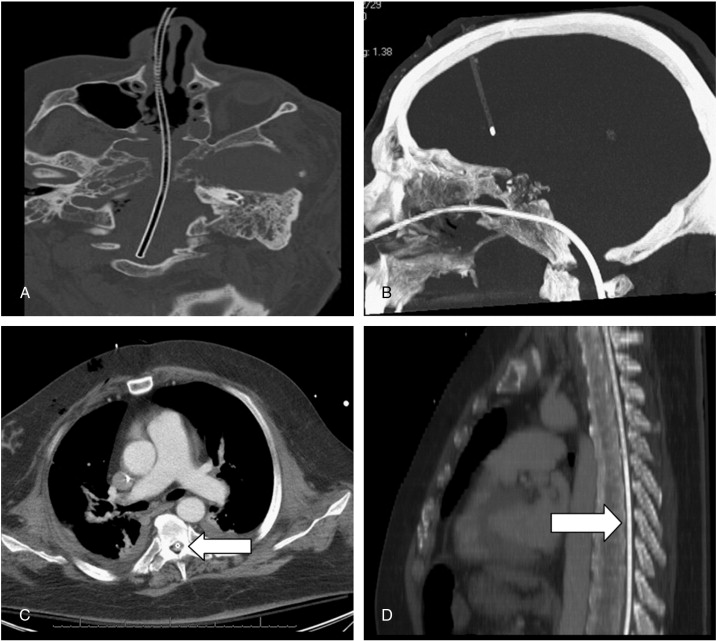
Kalitan's attorneys said anesthesia was used to put her "to sleep" for the outpatient carpal-tunnel surgery. When she awoke, she complained of chest and back pain but was later sent home. She was rushed to the hospital the next day, with an infection from the perforated esophagus and had to undergo chest and neck surgery. She was place in a drug-induced coma for three weeks while recovering.
A jury awarded Kalitan about $4.7 million, with $4 million of that in non-economic damages, according to court records. But a circuit judge, applying the caps from the 2003 law, reduced the non-economic damages award by about $2 million, which included a finding that Kalitan suffered a "catastrophic injury.""
"A South Florida appeals court ruled last week that the law's limits on pain and suffering damages — known in legal parlance as non-economic damages — are unconstitutional in personal-injury cases, such as the case of Susan Kalitan, who was injured after tubes were inserted into her mouth and esophagus as part of an anesthesia process."
Court ruling a new blow to Florida's medical-malpractice damage caps
Whelp.
Kalitan filed the malpractice case in 2008 in Broward County and named a series of defendants, including the North Broward Hospital District, an anesthesiologist, a certified registered nurse anesthetist and a company that contracted to provide anesthesiologists and staff to the hospital district.
Kalitan's attorneys said anesthesia was used to put her "to sleep" for the outpatient carpal-tunnel surgery. When she awoke, she complained of chest and back pain but was later sent home. She was rushed to the hospital the next day, with an infection from the perforated esophagus and had to undergo chest and neck surgery. She was place in a drug-induced coma for three weeks while recovering.
A jury awarded Kalitan about $4.7 million, with $4 million of that in non-economic damages, according to court records. But a circuit judge, applying the caps from the 2003 law, reduced the non-economic damages award by about $2 million, which included a finding that Kalitan suffered a "catastrophic injury.""
"A South Florida appeals court ruled last week that the law's limits on pain and suffering damages — known in legal parlance as non-economic damages — are unconstitutional in personal-injury cases, such as the case of Susan Kalitan, who was injured after tubes were inserted into her mouth and esophagus as part of an anesthesia process."
Court ruling a new blow to Florida's medical-malpractice damage caps
Whelp.