- Joined
- Nov 18, 2002
- Messages
- 5,220
- Reaction score
- 2,435
This great study from BMJ just came out:
http://www.bmj.com/content/356/bmj.j239
Objective To measure incidence of early death after discharge from emergency departments, and explore potential sources of variation in risk by measurable aspects of hospitals and patients.
Design Retrospective cohort study.
Setting Claims data from the US Medicare program, covering visits to an emergency department, 2007-12.
Participants Nationally representative 20% sample of Medicare fee for service beneficiaries. As the focus was on generally healthy people living in the community, patients in nursing facilities, aged ≥90, receiving palliative or hospice care, or with a diagnosis of a life limiting illnesses, either during emergency department visits (for example, myocardial infarction) or in the year before (for example, malignancy) were excluded.
Main outcome measure Death within seven days after discharge from the emergency department, excluding patients transferred or admitted as inpatients.
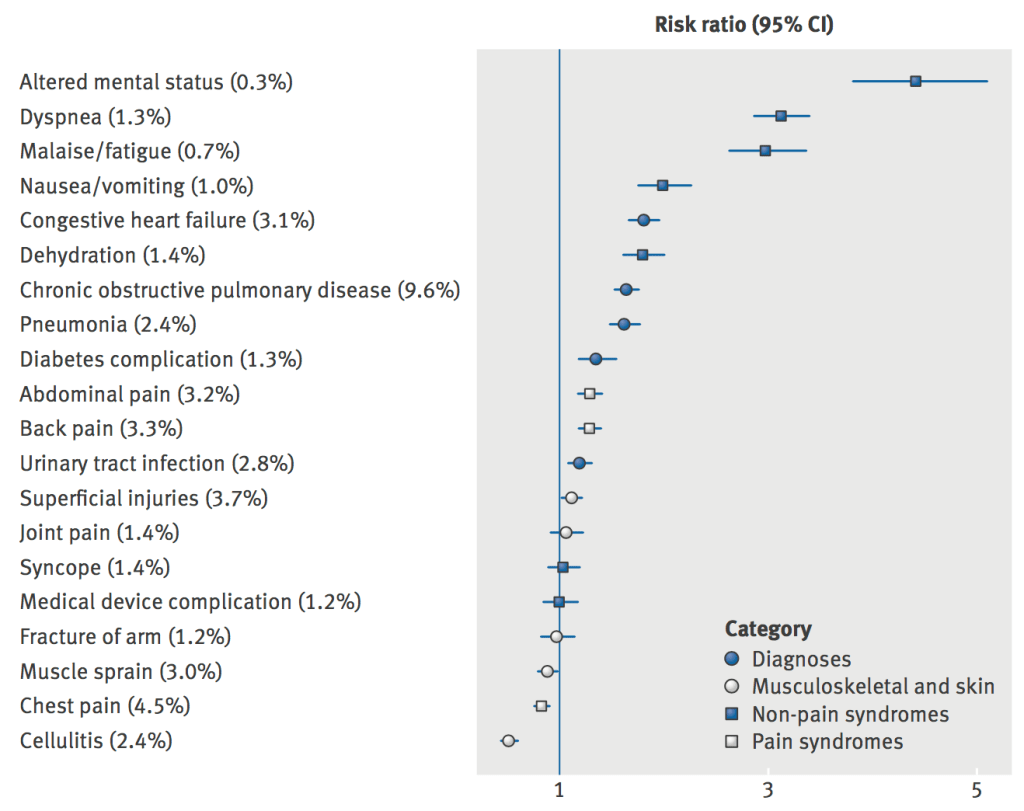
Results Among discharged patients, 0.12% (12 375/10 093 678, in the 20% sample over 2007-12) died within seven days, or 10 093 per year nationally. Mean age at death was 69. Leading causes of death on death certificates were atherosclerotic heart disease (13.6%), myocardial infarction (10.3%), and chronic obstructive pulmonary disease (9.6%). Some 2.3% died of narcotic overdose, largely after visits for musculoskeletal problems. Hospitals in the lowest fifth of rates of inpatient admission from the emergency department had the highest rates of early death (0.27%)—3.4 times higher than hospitals in the highest fifth (0.08%)—despite the fact that hospitals with low admission rates served healthier populations, as measured by overall seven day mortality among all comers to the emergency department. Small increases in admission rate were linked to large decreases in risk. In multivariate analysis, emergency departments that saw higher volumes of patients (odds ratio 0.84, 95% confidence interval 0.81 to 0.86) and those with higher charges for visits (0.75, 0.74 to 0.77) had significantly fewer deaths. Certain diagnoses were more common among early deaths compared with other emergency department visits: altered mental status (risk ratio 4.4, 95% confidence interval 3.8 to 5.1), dyspnea (3.1, 2.9 to 3.4), and malaise/fatigue (3.0, 2.9 to 3.7).
Conclusions Every year, a substantial number of Medicare beneficiaries die soon after discharge from emergency departments, despite no diagnosis of a life limiting illnesses recorded in their claims. Further research is needed to explore whether these deaths were preventable.
They controlled for what you would expect is causing this.
My conclusion? Admit all Medicare patients no matter what they came in with. Then they'll die within 7 days of hospital discharge instead of ED discharge. I wish they had more of a discussion about what an acceptable 7 day death rate was, because 0% isn't happening.
http://www.bmj.com/content/356/bmj.j239
Objective To measure incidence of early death after discharge from emergency departments, and explore potential sources of variation in risk by measurable aspects of hospitals and patients.
Design Retrospective cohort study.
Setting Claims data from the US Medicare program, covering visits to an emergency department, 2007-12.
Participants Nationally representative 20% sample of Medicare fee for service beneficiaries. As the focus was on generally healthy people living in the community, patients in nursing facilities, aged ≥90, receiving palliative or hospice care, or with a diagnosis of a life limiting illnesses, either during emergency department visits (for example, myocardial infarction) or in the year before (for example, malignancy) were excluded.
Main outcome measure Death within seven days after discharge from the emergency department, excluding patients transferred or admitted as inpatients.
Results Among discharged patients, 0.12% (12 375/10 093 678, in the 20% sample over 2007-12) died within seven days, or 10 093 per year nationally. Mean age at death was 69. Leading causes of death on death certificates were atherosclerotic heart disease (13.6%), myocardial infarction (10.3%), and chronic obstructive pulmonary disease (9.6%). Some 2.3% died of narcotic overdose, largely after visits for musculoskeletal problems. Hospitals in the lowest fifth of rates of inpatient admission from the emergency department had the highest rates of early death (0.27%)—3.4 times higher than hospitals in the highest fifth (0.08%)—despite the fact that hospitals with low admission rates served healthier populations, as measured by overall seven day mortality among all comers to the emergency department. Small increases in admission rate were linked to large decreases in risk. In multivariate analysis, emergency departments that saw higher volumes of patients (odds ratio 0.84, 95% confidence interval 0.81 to 0.86) and those with higher charges for visits (0.75, 0.74 to 0.77) had significantly fewer deaths. Certain diagnoses were more common among early deaths compared with other emergency department visits: altered mental status (risk ratio 4.4, 95% confidence interval 3.8 to 5.1), dyspnea (3.1, 2.9 to 3.4), and malaise/fatigue (3.0, 2.9 to 3.7).
Conclusions Every year, a substantial number of Medicare beneficiaries die soon after discharge from emergency departments, despite no diagnosis of a life limiting illnesses recorded in their claims. Further research is needed to explore whether these deaths were preventable.
They controlled for what you would expect is causing this.
My conclusion? Admit all Medicare patients no matter what they came in with. Then they'll die within 7 days of hospital discharge instead of ED discharge. I wish they had more of a discussion about what an acceptable 7 day death rate was, because 0% isn't happening.