- Joined
- Dec 18, 2015
- Messages
- 3,217
- Reaction score
- 4,930
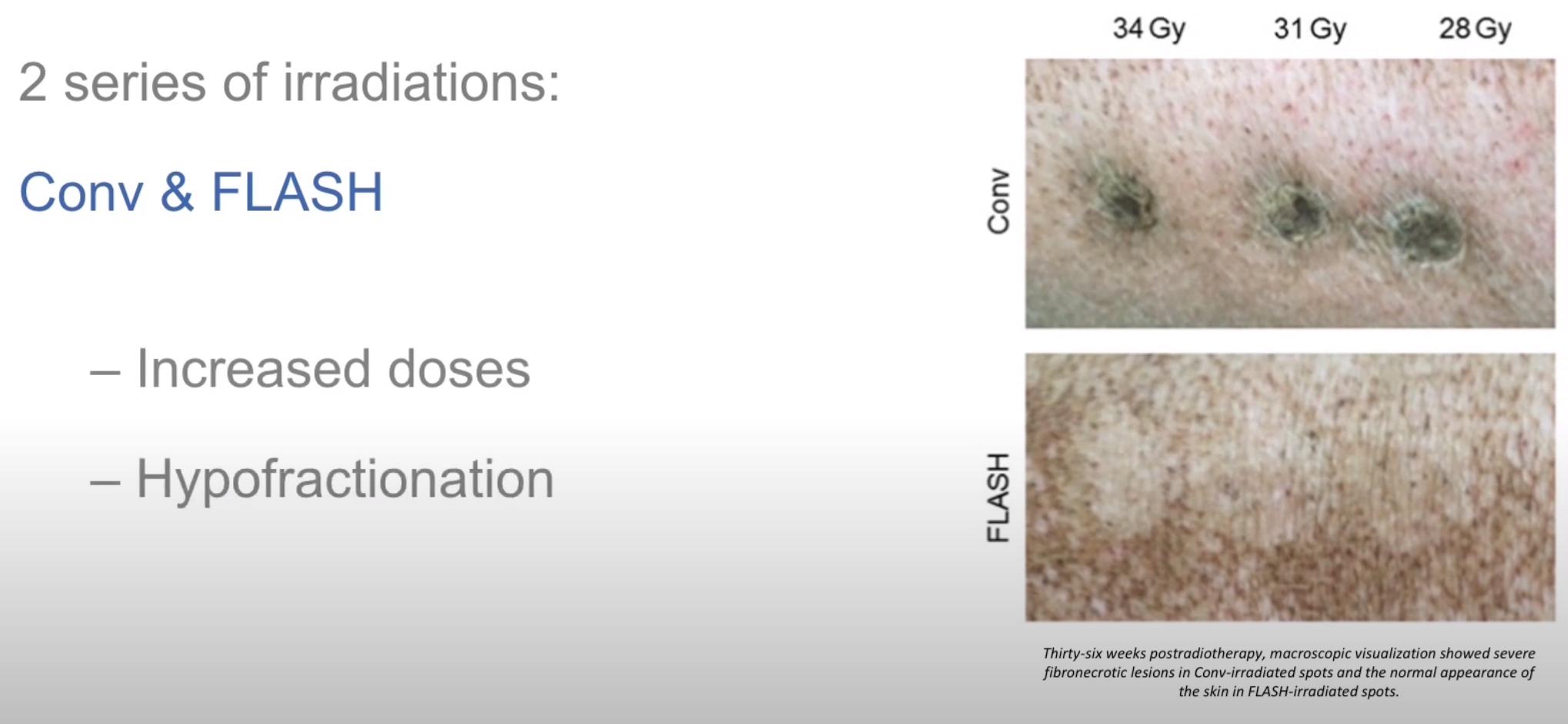
FLASHKNiFE: the FLASH Radiotherapy System | PMB from technology to innovation
Radiotherapy has been used for several decades to treat cancer and intensive research has made it a powerful and precise treatment for patients today. Although it has dramatically improved over the years, the efficiency of conventional radiotherapy is still limited by the complications and...
I'm upping the odds on FLASH. If it all follows to the hinted-at logical conclusions, this could have some very (scary? existential?) important implications:
1) Radiotherapies (most?) in single sessions
2) Less need for "clinical hand-holding" due to diminished side effects, OARs will be antiquated notions e.g.
3) Much technology on IGRTing and motion tracking etc will be antiquated notions too
4) The radiobiology we learn today will have no application to clinical practice, the rules will need to be re-written, Hall thrown out, etc., and in essence there will be no "rules" per se (no cord tolerance concept e.g.?) because the radiation will be so safe
5) Others? Workforce (of course)?