- Joined
- Dec 17, 2007
- Messages
- 3,796
- Reaction score
- 5,427
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
I do not think there's a role for RT in resectable, small cT1-2 cN0 pancreatic cancer. These patients should get surgery and perioperative chemotherapy. It will be impossible to prove that RT plays a role here, noone will peform a randomized trial and some would even suggest that randomizing patients between the standard of care and "experimental RT" would be unethical, actually.
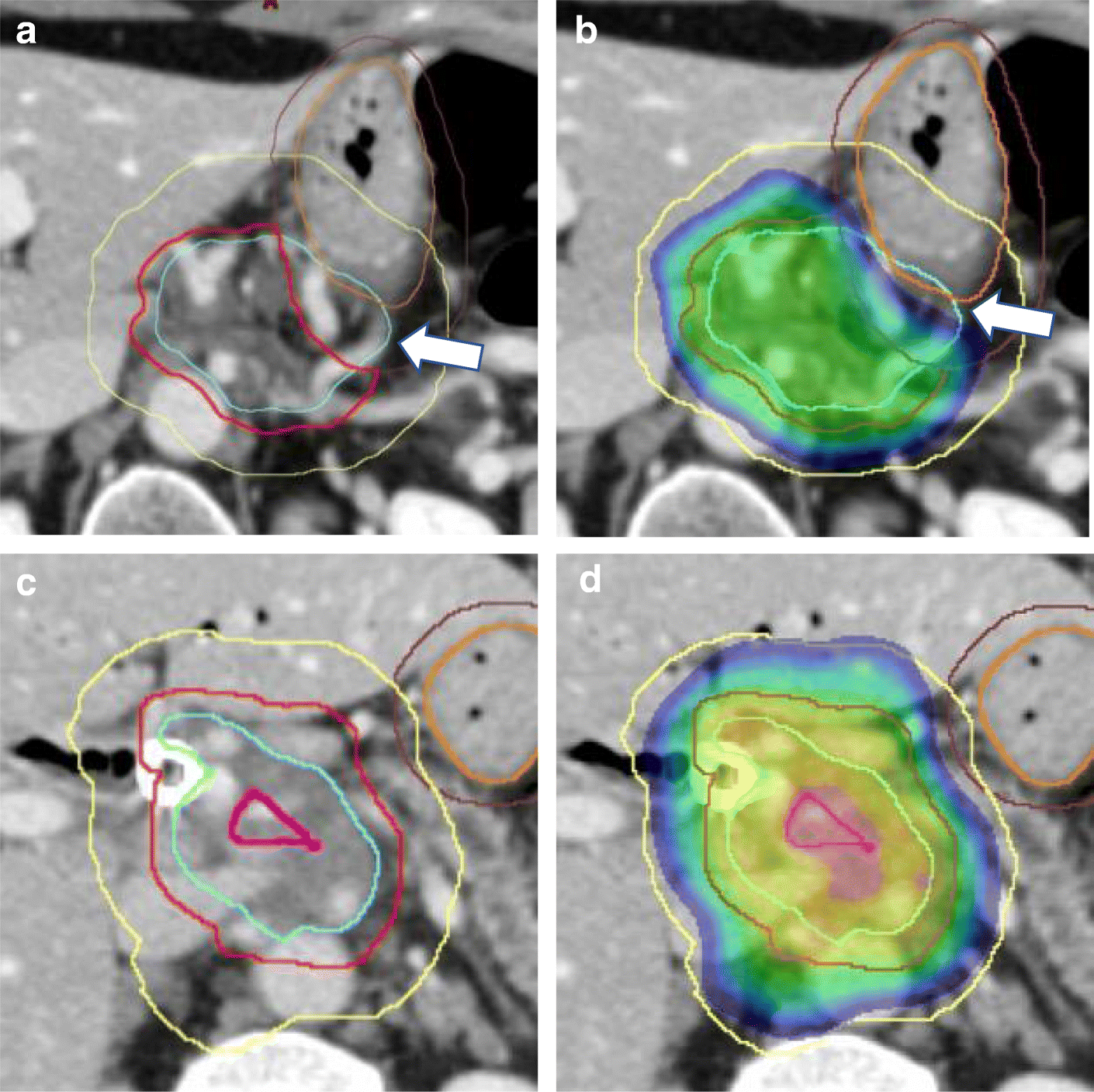
The problem is that many physicians, mainly surgeons, extrapolate from these results and advocare for surgery as a must in cT3-cT4 or cN+ disease. Whether or not surgery truly improves survival in these patients or these patients are basically doomed to reccur and die anyway, with surgery adding very little in terms of OS and even then with significant morbidity, is debateable. This is the space, where perhaps RT together with systemic therapy can play a role. The problem here however is, that many of these patients are not eligible for "Crane"-approaches, since these tumors are big and one cannot meet constraints for duodenum without underdosing the GTV.
It's a complicated matter...
The problem is that many physicians, mainly surgeons, extrapolate from these results and advocare for surgery as a must in cT3-cT4 or cN+ disease. Whether or not surgery truly improves survival in these patients or these patients are basically doomed to reccur and die anyway, with surgery adding very little in terms of OS and even then with significant morbidity, is debateable. This is the space, where perhaps RT together with systemic therapy can play a role. The problem here however is, that many of these patients are not eligible for "Crane"-approaches, since these tumors are big and one cannot meet constraints for duodenum without underdosing the GTV.
It's a complicated matter...