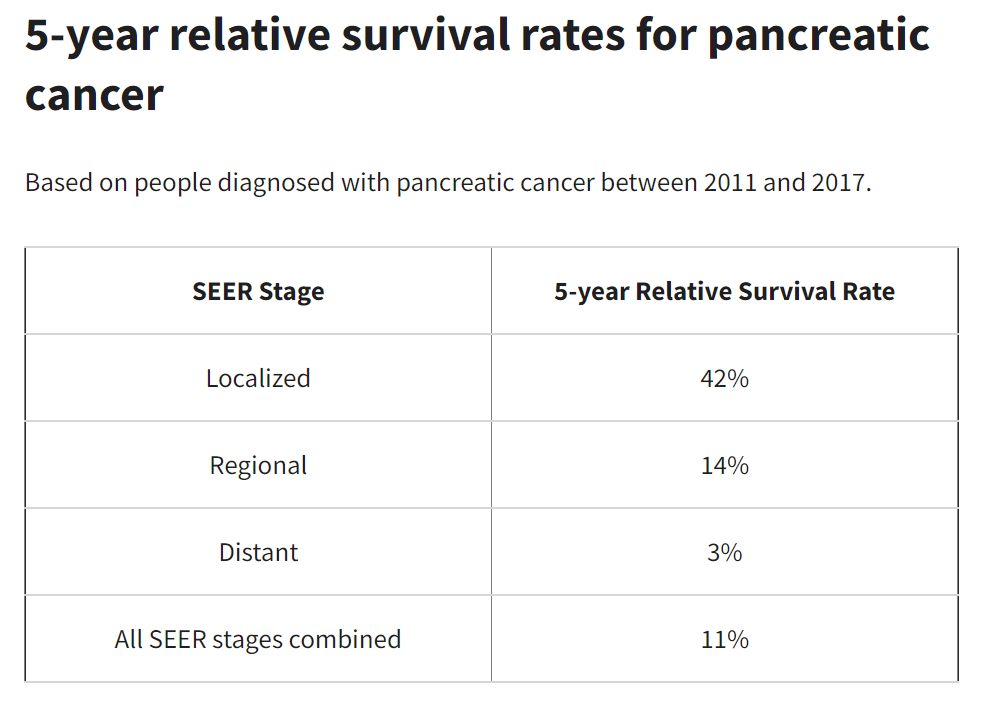
Yeah, in this universe, unresectable will never approach the survival of resectable. But correct me if I'm wrong
@bigman1, that was not your premise. I think the premise of the OP was flawed ("I thought overall survival was less than 20% at 5 year mark for all stages head of pancreas"). While resectable pancreatic adenoCA is itself a not common entity, within that group long-term survivors are not
that uncommon (if you believe the
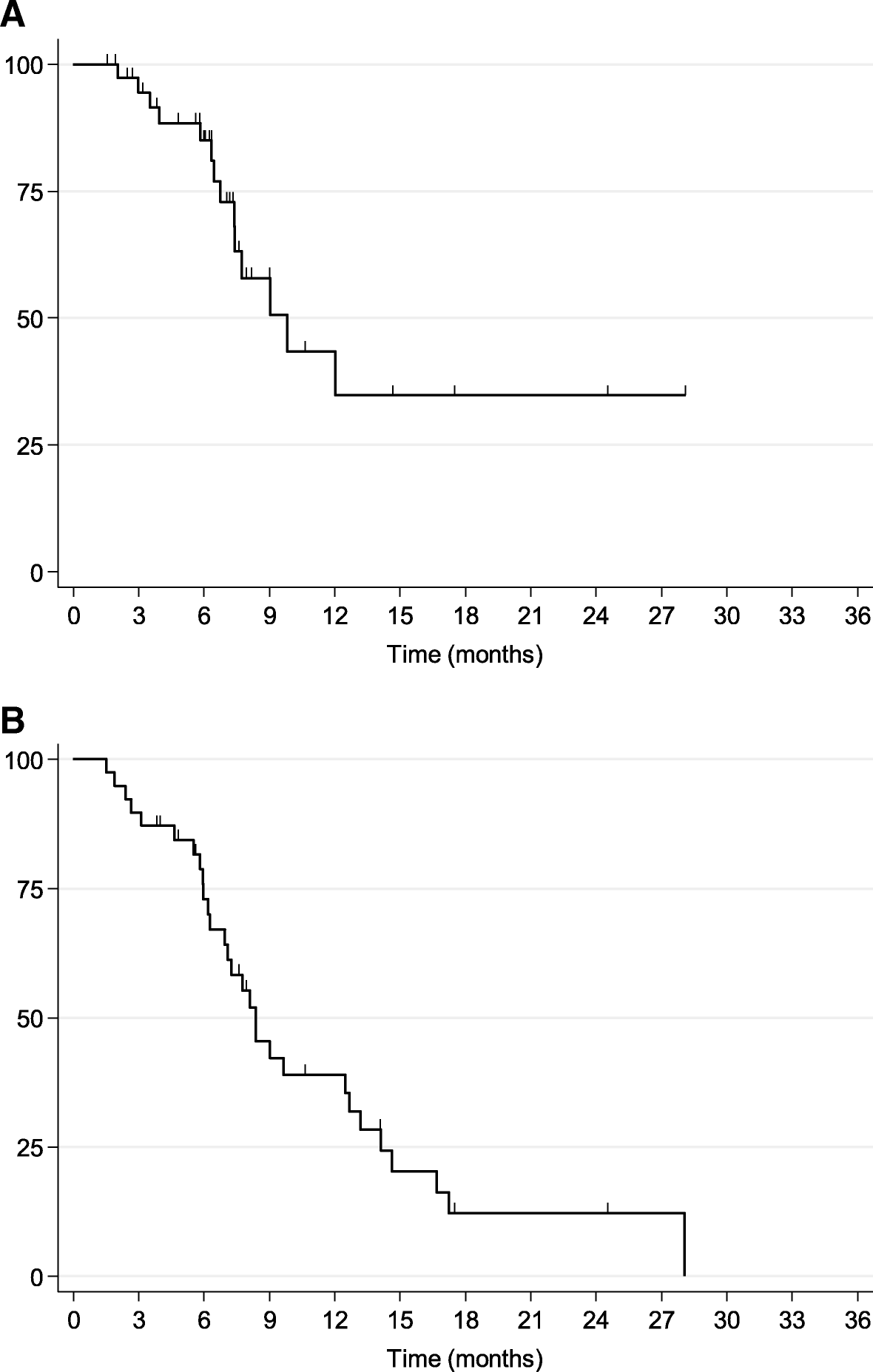
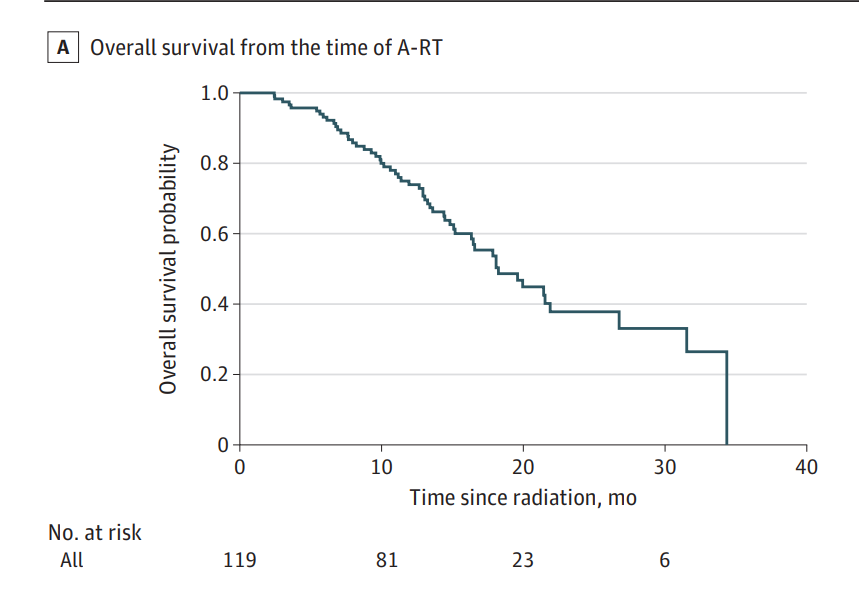
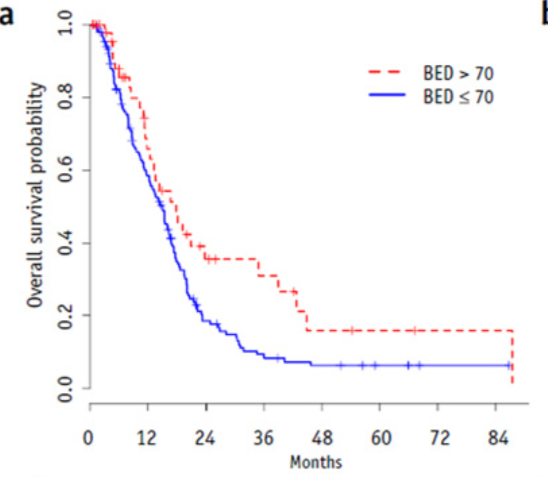
American Cancer Society e.g.). Not to be a wet dishrag, but the 95% C.I. on that 31% 3y OS would overlap with published chemo-only or chemoRT survivals (roughly only about 10 patients in the BED>70 arm were available for events/censoring by the 3y mark and were the basis for the 31% metric).