- Joined
- Jan 18, 2013
- Messages
- 152
- Reaction score
- 15
Dear colleagues,
your opinion is highly appreciated:
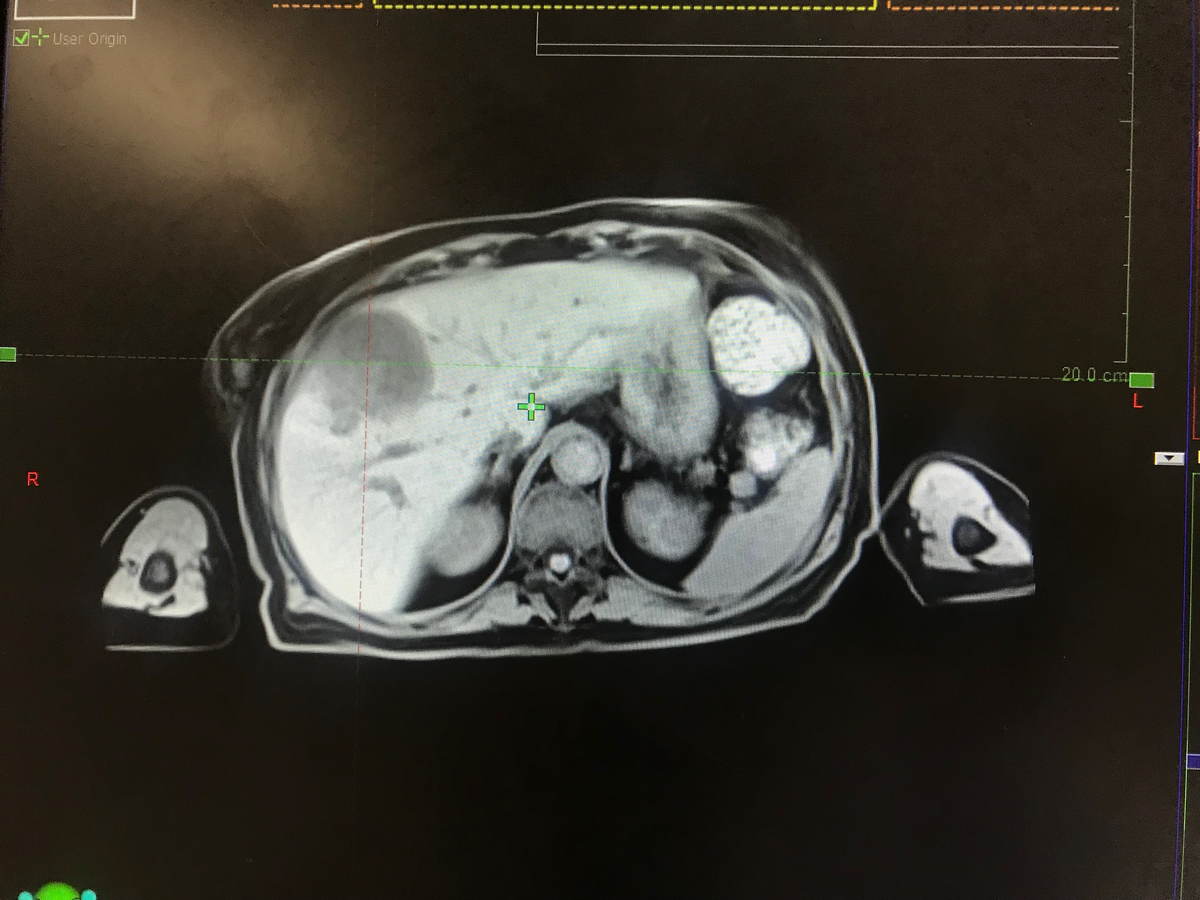
55 years old female, diagnosed of a pancreatic adenocarcinoma in 2017. She underwent a Whipple surgery followed by adjuvant chemoradiation to the tumor bed using a 3 fields 3D-conformal plan.
In 2019, she developed a single liver lesion of 2.5 cm , segment VIII treated with RFA.
3 months after, the lesion progressed in size reaching 7 cm , CA19-9 5000, with no other secondary lesion elsewhere.
Her liver function is maintained, only GGT and ALP are elevated.
Screenshots of her MRI and delineated CT sim are attached below.
GTV acc volume: 291 cc
PTV volume: 436 cc
Liver-GTVacc volume: 1000 cc
Is Iiver SBRT an option?
What dose and fractionation do you recommend?


your opinion is highly appreciated:
55 years old female, diagnosed of a pancreatic adenocarcinoma in 2017. She underwent a Whipple surgery followed by adjuvant chemoradiation to the tumor bed using a 3 fields 3D-conformal plan.
In 2019, she developed a single liver lesion of 2.5 cm , segment VIII treated with RFA.
3 months after, the lesion progressed in size reaching 7 cm , CA19-9 5000, with no other secondary lesion elsewhere.
Her liver function is maintained, only GGT and ALP are elevated.
Screenshots of her MRI and delineated CT sim are attached below.
GTV acc volume: 291 cc
PTV volume: 436 cc
Liver-GTVacc volume: 1000 cc
Is Iiver SBRT an option?
What dose and fractionation do you recommend?

