I am reading the "Inhalation Anesthetics" chapter in Clinical Anesthesiology for my anesthesia rotation and found myself confused on the topic of factors affecting alveolar concentration.
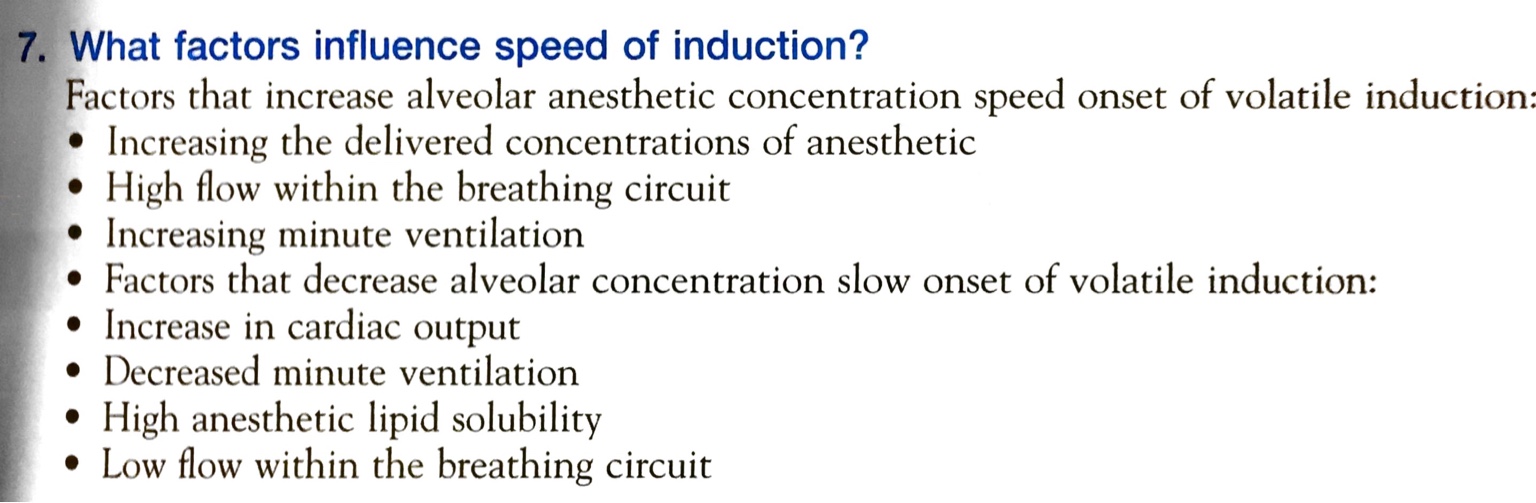
How is it that an INCREASE in cardiac output, which increases the uptake of the anesthetic, actually DELAYS the induction and a DECREASE in cardiac output can actually lead to OVERDOSAGE of anesthetics?
I understand that the partial pressure difference between alveolar gas and venous blood, and the solubility in blood affect the uptake, but cannot seem to wrap my brain why an increase in alveolar blood flow slows induction?
Any help?
How is it that an INCREASE in cardiac output, which increases the uptake of the anesthetic, actually DELAYS the induction and a DECREASE in cardiac output can actually lead to OVERDOSAGE of anesthetics?
I understand that the partial pressure difference between alveolar gas and venous blood, and the solubility in blood affect the uptake, but cannot seem to wrap my brain why an increase in alveolar blood flow slows induction?
Any help?