- Joined
- Jul 9, 2007
- Messages
- 1,199
- Reaction score
- 243
I've seen the back and forth controversy regarding nerve blocks for humerus, radial/ulnar fx. mike stone does it without any problems. ortho of course gets upset and brings up the whole compartment syndrome issue. if the pt is getting lido only which will wear off by 4 hrs, isn't it pretty safe?
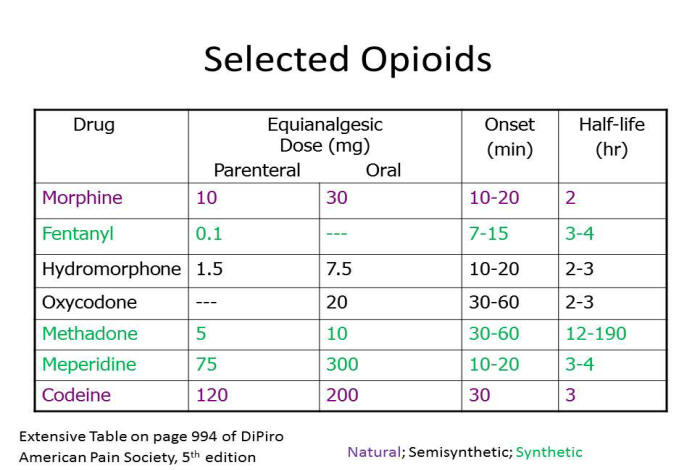
we're converting to a dilaudid and perco-snack free ED so I am trying to give some alternatives
we're converting to a dilaudid and perco-snack free ED so I am trying to give some alternatives