HIV+ 60 yo male with severe BLE radicular pain for 5 months. Fell off a ladder in his garage and had immediate severe back and BLE pain. No prior episodes of pain or really any medical issues other than well controlled HIV.
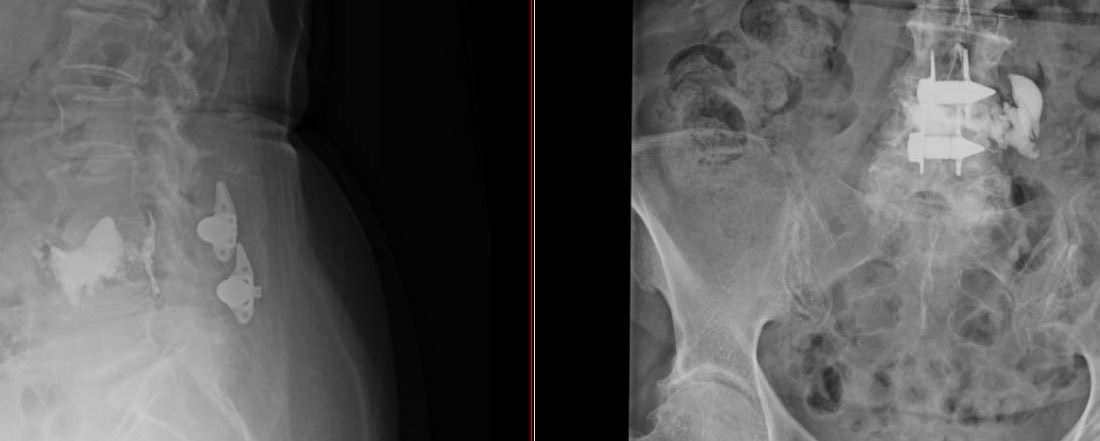
After falling off the ladder he presented to the ED who did an XRAY, ruled out fracture, gave toradol, and sent home with tramadol. Presented to the ED again a few days later, and this went on for a few weeks.
Referred to a local pain clinic who did basically nothing for him for 4 months. No imaging. No Rx. Some of these details I don't remember, but basically they did nothing for like 4 months. Definitely no scans or even gabapentin.
I open the door to the exam room and find a pleasant gentleman who can't sit still and is pouring sweat, plus he appears somewhat cachectic and generally feeble. I can't do an exam bc he is in severe pain, but I don't feel like he is histrionic or emotionally labile. He feels legit to me.
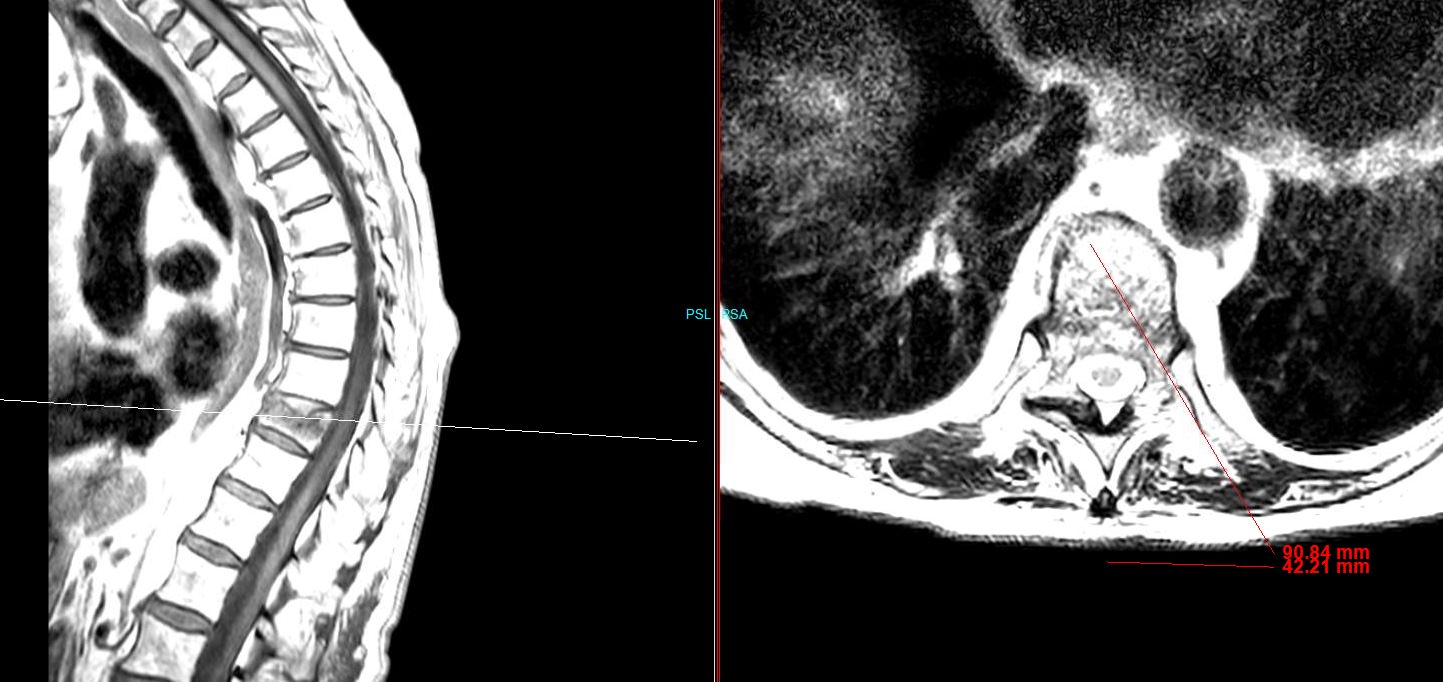
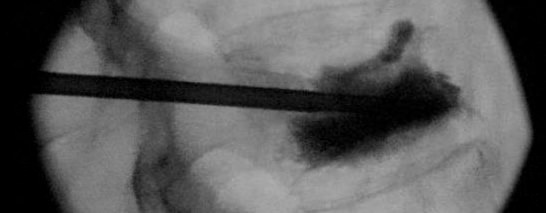
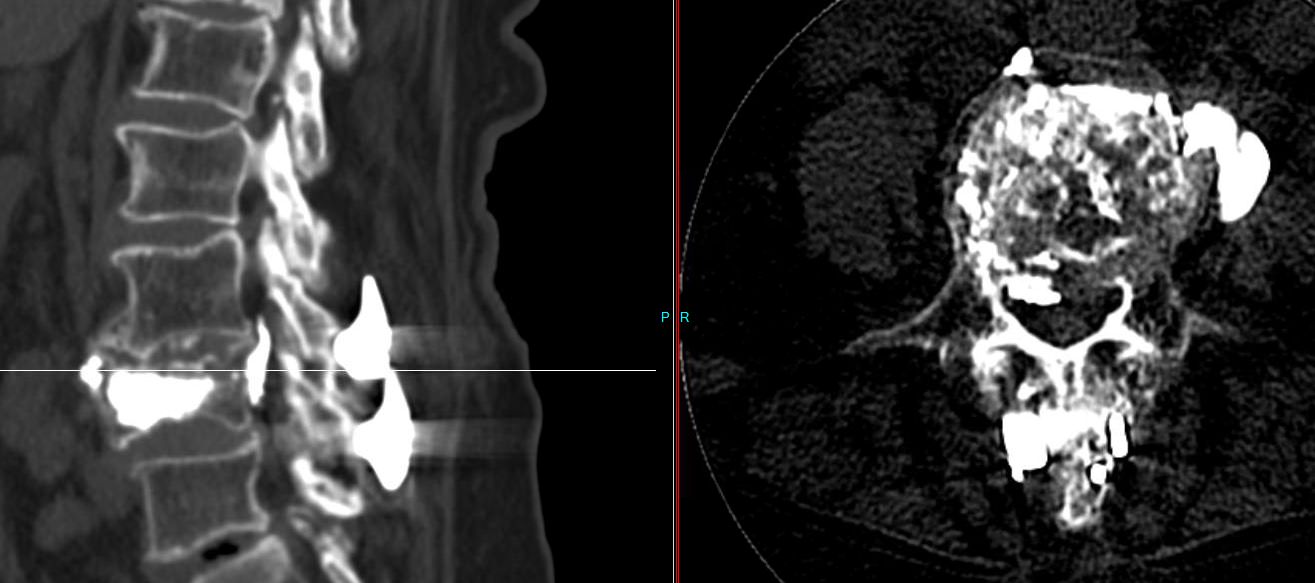
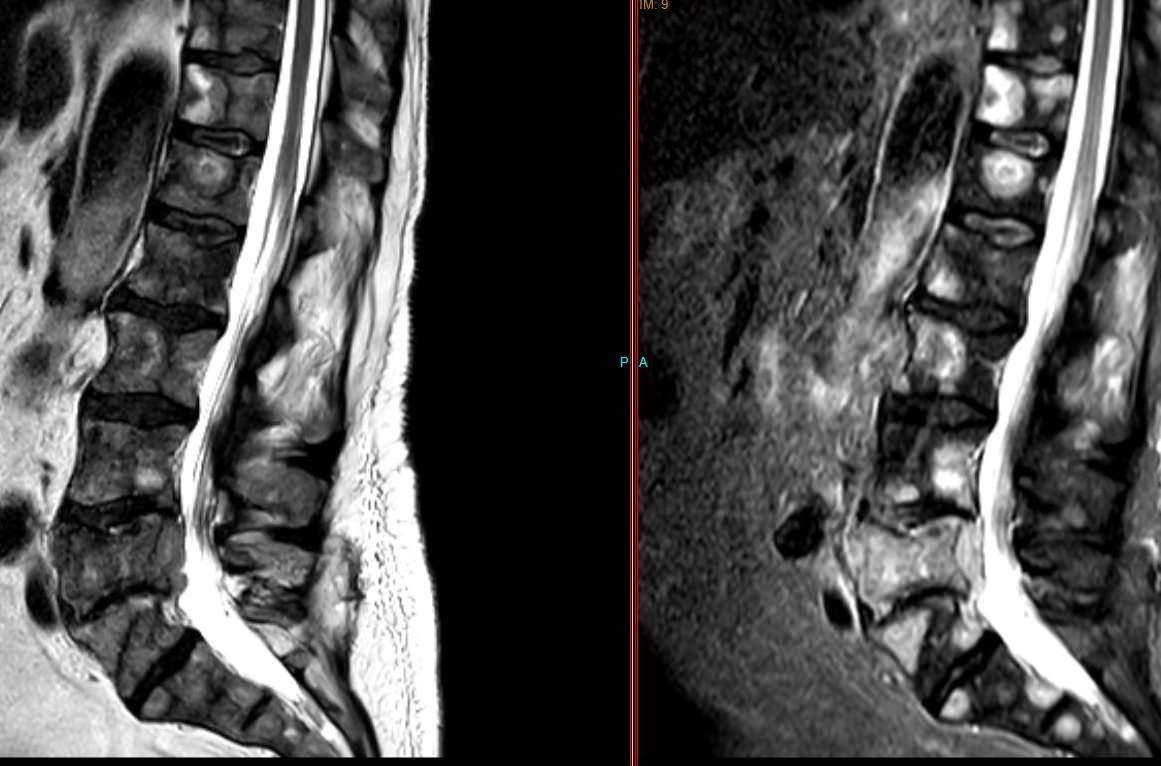
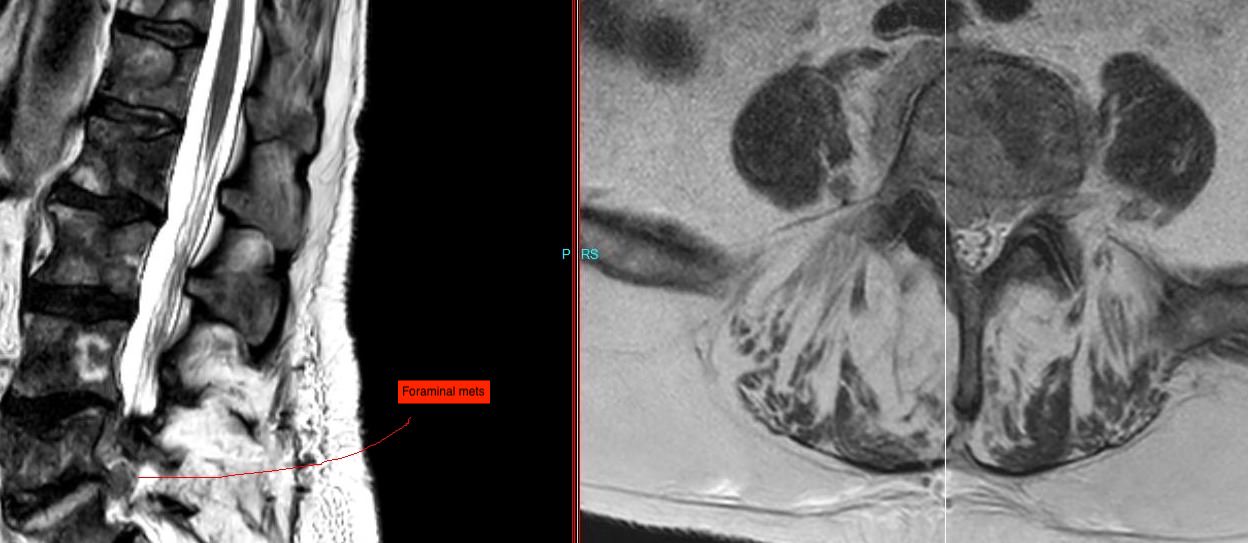
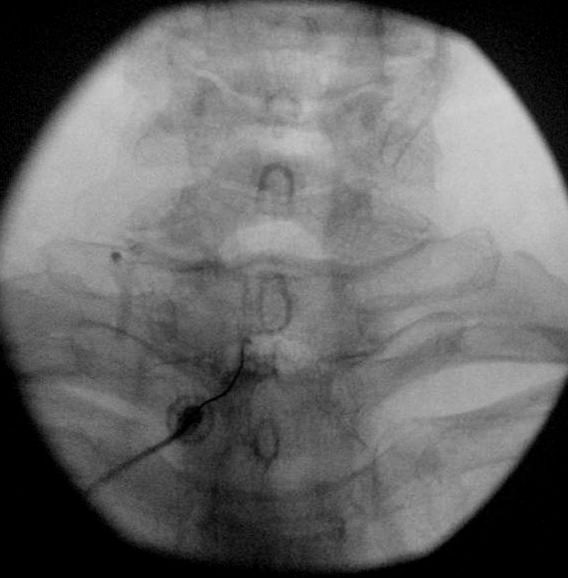
I send him for an MRI and here are two pics from that scan. These images basically sum up L3 to the sacrum.
I bring him in to tell him he may have cancer and direct him to the ED for a workup.
I haven't seen or heard from him since then, and this was 4 months ago.
Moral of the story - Get a damn MRI on a diaphoretic and cachectic male with HIV and severe pain.