- Joined
- Oct 3, 2014
- Messages
- 390
- Reaction score
- 467
I came across this graph, which I think med students and junior residents may find useful for patient workup or counseling their patients about radiation risk from diagnostic imaging tests with ionizing radiation.
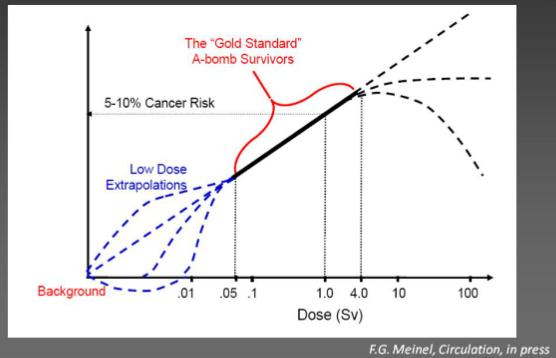
Chest radiograph: ~0.1 mSv
CT abdomen and pelvis: ~10 mSv
The x-axis in the graph above is in Sv. Both tests fall into the "low dose extrapolation" region.
A lot of "radiation risk" discussions at the ordering level are based on vague presentiments based on click-bait ramblings from the New York Times. It's always prudent to use a dose as low as reasonable to accomplish the diagnostic need... but a graph is worth a lot of misguided hearsay in terms of what we actually know and don't know about radiation risk.
Can we prove that diagnostic-level radiation is harmless? No.
Can we prove it is harmful? No.
Is getting a CT going to give your patient cancer? Unlikely.
Should you get a CT? It depends on whether the benefit of the study outweighs the risk.
I imagine many already know this.
The only reason I put this up here is because I've come across some confusion about diagnostic radiation risk in recent discussions.
Chest radiograph: ~0.1 mSv
CT abdomen and pelvis: ~10 mSv
The x-axis in the graph above is in Sv. Both tests fall into the "low dose extrapolation" region.
A lot of "radiation risk" discussions at the ordering level are based on vague presentiments based on click-bait ramblings from the New York Times. It's always prudent to use a dose as low as reasonable to accomplish the diagnostic need... but a graph is worth a lot of misguided hearsay in terms of what we actually know and don't know about radiation risk.
Can we prove that diagnostic-level radiation is harmless? No.
Can we prove it is harmful? No.
Is getting a CT going to give your patient cancer? Unlikely.
Should you get a CT? It depends on whether the benefit of the study outweighs the risk.
I imagine many already know this.
The only reason I put this up here is because I've come across some confusion about diagnostic radiation risk in recent discussions.

