- Joined
- Feb 24, 2018
- Messages
- 2,029
- Reaction score
- 1,160
Just for fun, can anyone explain the science side of this?
Last edited:
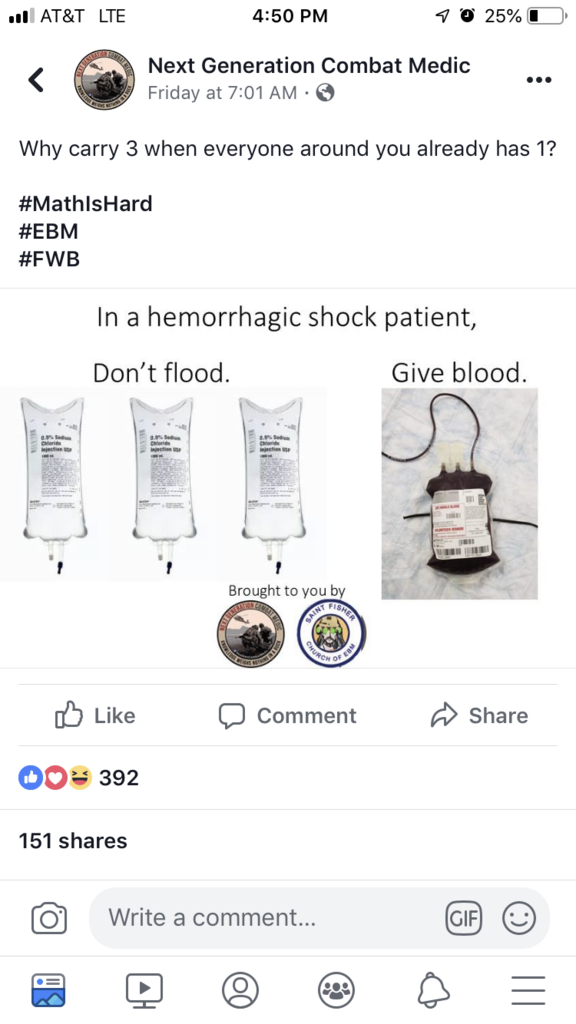
Where can premeds discuss things like that? I don’t think we can post in the attending forumsThis is the premed forum but in trauma 1:1:1 is now the gold standard. If you are giving fluids in the setting of hemorrhagic shock you are actively trying to kill someone.
We can’t post in the Practicing Physicians forum, but you can post in all of the other ones under Physicians/ResidentsWhere can premeds discuss things like that? I don’t think we can post in the attending forums
Can we move this to that forum please? Thank you mods
So, in a Combat Environment, if you are at a large enough CSH, the ‘walking blood bank’ protocol can be enacted. In theatre the blood bank does not fall under the FDA, so every soldier stationed on the base will have extremsive antigen typing performed so that, in the event of a mass casualty or severe trauma scenario, whole-blood transfers can be utilized."everyone around you already has 1"
Does that mean infantrymen carry 1L of saline each, typically?
The craziest trauma I've ever done was on a liver cirrhotic patient that was involved in a MVA. 43 pRBCs, 27 FFP, 4 platelets and 20 cryo initially then came back a few hours later and got another 13/15/1/20.
Just wondering how big a part Cell Saver / autologous transfusion plays in trauma? I know it gets used a lot for scheduled/elective surgeries where blood loss is anticipated, but does it just take too long to set up or not work fast enough to keep up with blood loss in a case like this? It must be maddening to have so much blood end up on the floor/in a suction canister.
Several days? Man that’s fast.You can’t do autologous donations on a patient that doesn’t have blood in the first place...
In general, it will take several days to weeks for hematopoietic processes to replenish a unit of lost blood.
If anyone is curious of the time frame, the absolute minimum for the lab to do a room temp cross (which is even performed on O Neg...) is about 3 minutes plus transport and paperwork. A true type and cross takes about 15-20 minutes before the blood can be issued and a full work up is about an hour.I'm not military so I can't talk to the military trauma side of it but in traumas in general that come to the ORs I'll say a few things about how Anesthesia manages it. Can be slightly different than how the trauma surgeons like to do it. (albumin in trauma)
Findmeonthelink is correct that too much crystalloid does cause coagulation problems. Another thing to keep in mind is that crystalloids third space out so out of the 3L that you pump into someone about 1L remain in circulation after a certain amount of time. This can cause issues after the resuscitation is complete where you have airway edema (unable to extubate), dilutional coagulopathy, pulmonary edema, CHF exacerbation if the patient already has a compromised cardiac function. In massive traumas you should immediately check a DIC panel, specifically looking at the fibrinogen, to see if the patient is going towards DIC. Replacing with cryoprecipitate is the best for replacing fibrinogen. These MTP protocols can vary from hospital to hospital. Some do 6:6:1 but newer studies do say 1:1:1 is better. Ultimately, the main point is to keep resuscitating the patient until the bleeding is controlled and these situations tend to be chaotic and doesn't always flow as smoothly as you like. Sometimes blood bank sends the products off ratio, you lose track of how much of each product you've given when you're doing a million things at a time and the belmont is just going etc.
While blood in massive hemorrhagic shock is the best replacement, it does take the blood bank time to type and cross the patient's blood, thaw the blood/FFP/cryo for you to get it in. In the mean time you should definitely resuscitate with crystalloid in order to maintain some semblance of blood volume, perfusion pressure and oxygen delivery in the patient while you wait for the blood to come. Giving O neg also a possibility if you need it right away but the blood bank only has so much O neg that you can use at a time. The craziest trauma I've ever done was on a liver cirrhotic patient that was involved in a MVA. 43 pRBCs, 27 FFP, 4 platelets and 20 cryo initially then came back a few hours later and got another 13/15/1/20.
There's a technique called controllled hemodilution that you can do to minimize blood loss by diluting out the patient's blood so that it minimizes the disruption of oxygen carrying capacity of the hemoglobin when you do bleed. Not an appropriate technique in a massive trauma but a way to minimize the need for blood transfusions as they aren't without side effects.
Yah, for the first couple weeks the Hgb content will be decreased and the number of immature RBCs and WBCs (Reticulocytes banded neutrophils etc) will be increased.Several days? Man that’s fast.
Just wondering how big a part Cell Saver / autologous transfusion plays in trauma? I know it gets used a lot for scheduled/elective surgeries where blood loss is anticipated, but does it just take too long to set up or not work fast enough to keep up with blood loss in a case like this? It must be maddening to have so much blood end up on the floor/in a suction canister.
