Reimbursement, depending on how you want to define it, has held quite steady in rad onc for the last ~10y. But the "depending on how you want to define it" is the tricky part.
On a per code basis, reimbursement is maybe within 5% of its levels (if averaged per code) from 10y ago. BUT...some of the high dollar codes have gotten cut a lot, like IMRT for example. Many other factors too... e.g. 10y ago you could charge a complex treatment device for
every IMRT beam. CMS caught onto that and designed a whole new code called the "MLC device" that would be billed with IMRT no matter the beam number. That certainly cut reimbursement. And now CMS says no complex sim charges for IMRT or 3DCRT... a further cut in
TOTAL reimbursement. And there are numerous lines of evidence I have curated showing how total rad onc spending is flat or decreased (especially if you account for inflation) over the last 5-8y or so. That's remarkable when you think about it: there have been more new cancer patients per year and thus more new XRT patients per year. And the number of rad oncs, who initiate all rad onc reimbursement, is growing much faster than the preceding two things I mentioned.
But there has been pressure within to lower fraction numbers and from without to decrease XRT utilization over time. And high-tech treatments replacing old-style treatments don't usually reimburse more on a per patient basis. E.g., now that I'm doing 5-fx breast, not a single private payor is letting me bill SBRT for that. So you have a 5-fx IMRT course replacing what ~10y ago was a ~33fx IMRT or 3D course. (So I'm cutting my own reimbursement >50% in some cases.)
So why does CMS have a morbid fascination it seems with rad onc? In my opinion.... it all starts here.
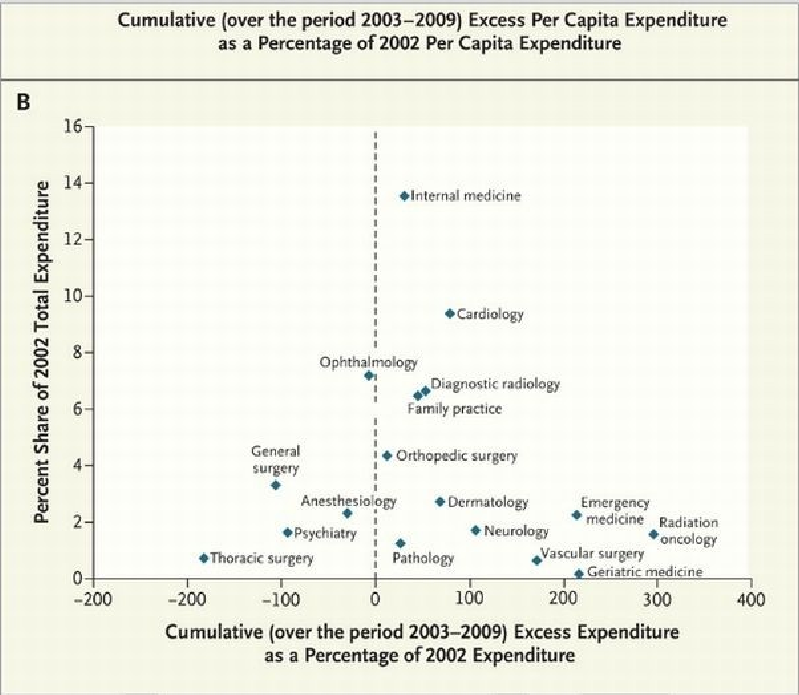
The NEJM published an article along about 2012 showing how rad onc had blown through the SGR, outpacing every specialty in America, over the 2003-09 time frame. For us rad oncs, it's easy to see why that happened. It was pure IMRT and a little IGRT thrown in on top. The number of patients treated with IMRT went from something like <5% to 50+% in those few years as IMRT became the definitive XRT of choice for most rad oncs. CMS didn't have the nuanced understanding necessary to see why rad onc had busted its SGR, and since that time CMS has been focused on rad onc. But it was this data primarily which got CMS' hackles up IMHO. (
Some might recall CMS once called for a ~40% cut to rad onc reimbursement.)
They should not be so rad onc-focused. And I think the back-away from the APM may signal that. And of course since ~2015, the SGR has been abolished. But I think the focus on rad onc is an inertia from the 2000-2010 time frame. Rad onc represents much less than 1% of all healthcare spending and about 7% (and declining) of all initial tx cancer spending (
recent data from Europe are similar to the US here). CMS understands math, but it is a govt monolith which is slow to react and also thus slow to "un-react." Again, I think we can predict CMS to "un-react" to rad onc in the future because 1) we are controlling our own costs, 2) cancer incidence is declining, and 3) all the other cancer cost centers outside rad onc are now the $ offenders.
(This is somewhat of a riff on "Voluntary residency contraction and the development of IMRT saved the field in the early 2000s: an analysis of the past 30 years.")