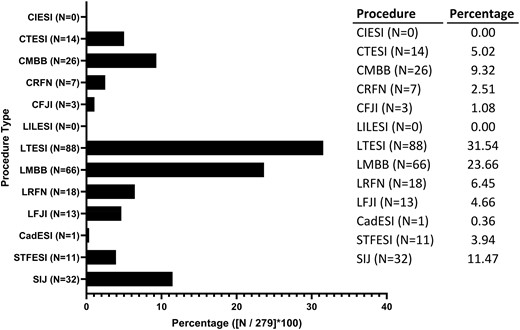
AbstractObjectives. To identify significant bleeding complications following spinal interventions in patients taking medications with antiplatelet or anticoagul

academic.oup.com
AbstractObjectives. To determine prevalence rates of hemorrhagic complications in patients who either ceased or continued anticoagulants during interventio

academic.oup.com
Here is letter to editor after Endres 17 article:
Regarding the Safety of Interventional Pain Procedures in the Setting of Anticoagulation
Nafisseh S. Warner, MD,
Susan M. Moeschler, MD,
Jason S. Eldrige, MD
Pain Medicine, Volume 18, Issue 4, April 2017, Pages 819–820,
Regarding the Safety of Interventional Pain Procedures in the Setting of Anticoagulation
Published:
24 April 2017
Issue Section:
Letters to the Editor
Dear Editor,
The recent study by Endres and colleagues was read with great interest [
1]. It seeks to shed light on a very relevant topic—how can we safely provide pain interventions for the growing population of patients on antithrombotic therapy? While their experience is intriguing for pain interventionists, there are several considerations that merit further clarification.
First, details regarding the protocol for anticoagulation discontinuation are notably absent. As an example, when discontinuing warfarin, which patients received bridging therapy and how was bridging performed? It is well accepted that high-risk patients, including those with CHADS2 scores of 4 or higher [
2], recent venous thromboembolic disease [
3], and most mechanical heart valves [
3], are likely to require bridging therapy with unfractionated or low molecular weight heparin. The paucity of information about these essential patient-specific clinical characteristics makes it unclear whether thrombotic complications occurred in the setting of inadequate bridging or if they were due to unanticipated thrombosis in patients despite appropriate bridging therapy. These details are necessary before conclusions can be drawn regarding the safety of peri-procedural antithrombotic use, at least in terms of understanding the true relative risks of thrombotic complications when discontinuing vs continuing warfarin therapy. Similar considerations apply to those on antiplatelet agents (e.g., clopidogrel, aspirin/dypridamole) following percutaneous coronary interventions or acute intracranial ischemic events.
Second, while this study is large in size, it is actually quite small in relation to the estimated incidence of bleeding complications following such procedures. For example, in the regional anesthesia literature, the incidence of epidural hematoma is estimated to be approximately one to two for every 100,000 procedures [
4]. Assuming a similar bleeding rate for interventional pain procedures, this study is significantly underpowered to provide definitive commentary on the risk of bleeding events, regardless of the presence or absence of anticoagulant therapy. Additionally, details regarding the definition of complications or “adverse effects” would benefit from further clarification. What constituted an adverse effect—bleeding requiring evaluation in the emergency department, motor deficits requiring urgent neurologic evaluation, or perhaps drops in hemoglobin concentration?
Third, it would greatly enhance the study’s impact to report preprocedural international normalized ratio (INR) values. One must recall that INR is not a simple linear scale that directly reflects the severity of anticoagulation. Rather, the INR is a nonlinear, exponential scale primarily sensitive to changes in factor VII levels [
5]. As such, one may anticipate marked differences in factor level activity despite seemingly small changes in INR (e.g., comparing INR values of 2 and 3); this, in turn, likely correlates with bleeding risk. With nearly 5,000 procedures performed, reporting of the preprocedural INR values would be of great clinical relevance.
In summary, the work presented by Endres and colleagues is a notable addition to the pain medicine literature, and we applaud the authors for their efforts. However, clinicians require further information regarding this patient population. Additional studies are needed to clarify risks and benefits for patients on antithrombotic therapy undergoing interventional procedures. Specifically, it is unlikely that simple continuation of antithrombotic medications is a “one-size-fits-all” answer to this complicated issue. Further study is needed to identify those patients best served by antithrombotic discontinuation and how to do so safely.
Funding sources: No funding sources were used to support this manuscript.
Conflicts of interest: None.
References
1
Endres
S
,
Shufelt
A
,
Bogduk
N.
The risks of continuing or discontinuing anticoagulants for patients undergoing common interventional pain procedures
.
Pain Med
2017
;18:403–409.
Google Scholar
2
Wysokinski
WE
,
McBane
RD
,
Daniels
PR
, et al. .
Periprocedural anticoagulation management of patients with nonvalvular atrial fibrillation
.
Mayo Clin Proc
2008
;
83
:
639
–
45
.
Google Scholar
Crossref
PubMed
3
Douketis
JD
,
Berger
PB
,
Dunn
AS
, et al. .
The perioperative management of antithrombotic therapy: American College of Chest Physicians evidence-based clinical practice guidelines (8th Edition)
.
Chest
2008
;
133
:
299S
–
339S
.
Google Scholar
Crossref
PubMed
4
Moen
V
,
Dahlgren
N
,
Irestedt
L.
Severe neurological complications after central neuraxial blockades in Sweden 1990-1999
.
Anesthesiology
2004
;
101
:
950
–
9
.
Google Scholar
Crossref
PubMed
5
Dzik
WH.
Predicting hemorrhage using preoperative coagulation screening assays
.
Curr Hematol Rep
2004
;
3
:
324
–
30
.
Google Scholar
PubMed
Response to above letter:
Response to Warner Letter
Stephen Endres, MD,
Nikolai Bogduk, MD
Pain Medicine, Volume 18, Issue 4, April 2017, Pages 820–821,
Response to Warner Letter
Published:
24 April 2017
Issue Section:
Letters to the Editor
Dear Editor,
For various reasons, it is not always possible to include in a manuscript all the details in which readers might be interested. The
Letterto the Editor section provides a means by which readers can ask for supplementary information, and by which authors can provide it.
Warner et al. cite a reference that provides an estimate of two in 100,000 for the prevalence of epidural hematoma. Warner N, Moeschler S, Eldrige J. Regarding the safety of interventional pain procedures in the setting of anticoagulation. Pain Med 2017;18:813–814. Of this we are aware, but the key feature is that this is an estimate; it is not a formal prospective count. We look forward to publications from anyone who can monitor 100,000 consecutive cases in order to produce a reliable count. Nevertheless, this “estimate” and the case reports to which we referred indicate that the risk of epidural hematoma following interlaminar procedures is not zero; and theoretically it would be greater in patients who are anticoagulated. Whether or not a risk of two in 100,000 is acceptable, especially for a procedure of contentious benefit, is an ethical question that bears consideration but is outside the brief of our published study. We do emphasize, however, that because of the reputed nonzero risk of hematoma, in no patient in our study did we continue anticoagulants during interlaminar injections.
Still in the realm of biostatistics, Warner et al. lament the small sample sizes in our study. This is why we reported 95% confidence intervals. These adjust the observed prevalence for sample size. It transpires that for procedures for which we had ample sample sizes we could statistically exclude a risk greater than 0.2%, viz. two in 1,000. To tighten these confidence intervals effectively to zero would require a study of 8,000 consecutive cases. For this we do not have the resources. However, our results serve to reassure would-be investigators that if they continue anticoagulants for spine pain procedures they are unlikely to encounter an epidemic of complications.
We did collect data on international normalized ratios. For patients in whom warfarin was continued, the mean value was 2.3, with a standard deviation of 0.6 and a range of 0.9 to 4.5. In those in whom warfarin was stopped, the values were 1.2 ± 0.4, with a range of 0.1 to 4.1. Remarkable in these values is the number of patients whose values were below or above the recommended therapeutic range, despite having been monitored by their treating physician. These aberrations underscore the importance of checking the patient’s value before embarking on a pain procedure, irrespective of whether or not warfarin is to be continued.
Our protocol for discontinuing anticoagulants was that, in all cases, the prescribing cardiologist decided whether the anticoagulant could be stopped or not, and how to stop it. At all times, the option obtained was retained of not performing the intended procedure.
Bridging therapy is a proposition that has not been explored in the context of spine pain procedures and was not entertained in our study. In essence, bridging therapy involves replacing a long-acting anticoagulant with frequently repeated doses of a short-acting agent, such as heparin, in order to provide a short window of opportunity during which the short-acting agent can be briefly withheld only for the duration of the procedure to be performed, after which the original agent can be reinstated. However, bridging therapy is tantamount to not ceasing anticoagulants. The thrust of our conclusions is that for innocuous procedures anticoagulants do not need to be ceased. Under those conditions, the original anticoagulant can be maintained, without the need for complex bridging therapy. It is only for interlaminar procedures that bridging therapy might be an entertainable intervention. However, it would be a demanding study that proved statistically that bridging therapy keeps the rate of complications to the estimated rate of two in 100,000.
With respect to adverse events, our patients were closely monitored, especially for serious complications in patients who continued anticoagulants. That monitoring allowed for collection of reports of other adverse events, such as troublesome local bleeding or non-neurologic complications that required medical attention, but none were reported.
We trust that this additional information reassures readers about our study and its conclusions. Common spine pain procedures have a low risk of serious hemorrhagic complications, which might be zero. On the other hand, ceasing anticoagulants has a low, but nonzero, risk of serious medical morbidity.
Summing it up: Both sides who know more than us have had the argument. Pick your winner.
If patient bleeds- you may get sued.
If patient has MI/CVA: you may get sued.
Weigh your risks vs benefits and roll those 150000 sided dice.