D
deleted1111261
How do your pathologists report out squamous cell cancer, particularly from head and neck?
We get:
1) the fact that it is squamous
2) margins negative or positive
Nothing else - no size, no PNI, no grade, no LVSI, no DOI. And, this is not the first place that does this. I have been at least 3 centers that report it out this way.
What do your pathologists do?
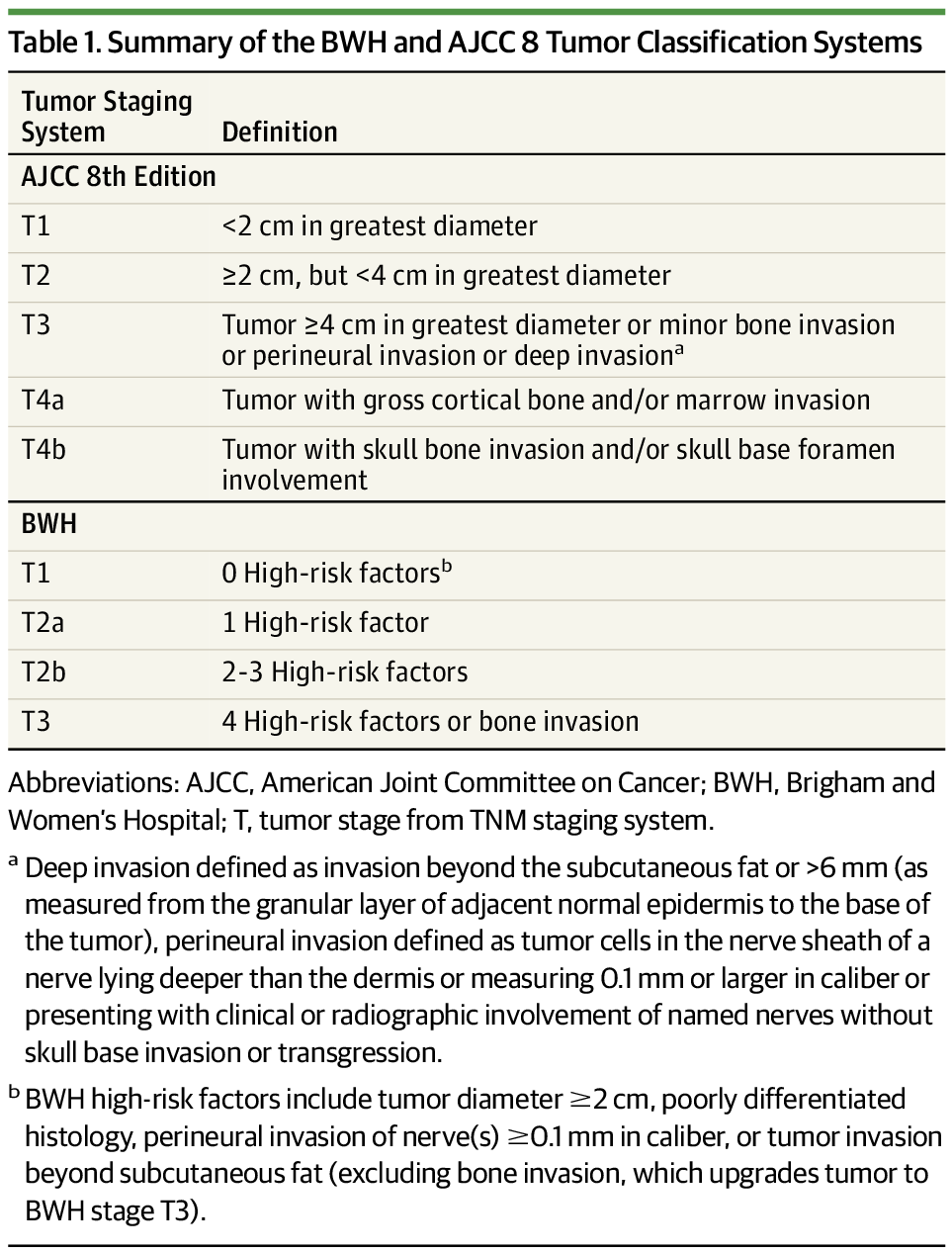
The CAP for squamous cell of the head and neck says all this should be reported out.
We get:
1) the fact that it is squamous
2) margins negative or positive
Nothing else - no size, no PNI, no grade, no LVSI, no DOI. And, this is not the first place that does this. I have been at least 3 centers that report it out this way.
What do your pathologists do?
The CAP for squamous cell of the head and neck says all this should be reported out.