- Joined
- May 15, 2009
- Messages
- 543
- Reaction score
- 6
OK, totally understand this is going to happen so I want to ask you all how you handle it. Awhile back I had a patient yelling at me and I said you need to lower your voice or I will call security. i think this escalated things. Pts family got more mad and then I left and called security. I noted another doc with a different philosophy which I liked. He says "i understand you are upset. i'm going to step out and give you a moment to compose yourself." and then reenter saying "are you ready to talk now?" Any thoughts on how you handle this? It's really difficult not to get angry when being yelled at and I think some tips on how to handle it would be helpful. we definitely don't learn this in medical school or residency.

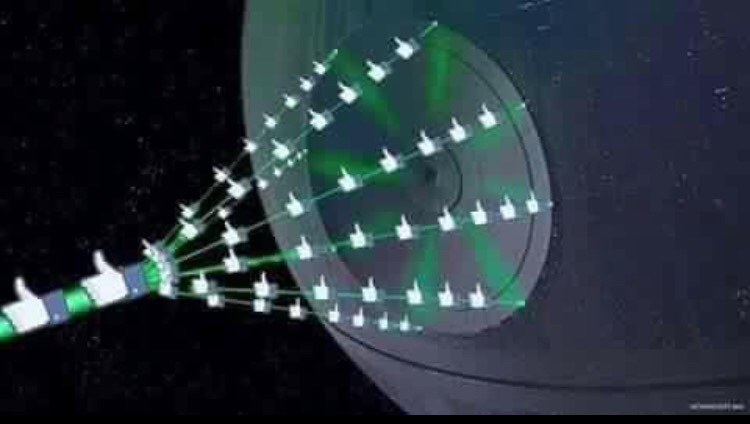
 likes onto my post with your Death Star-liker-laser?
likes onto my post with your Death Star-liker-laser?