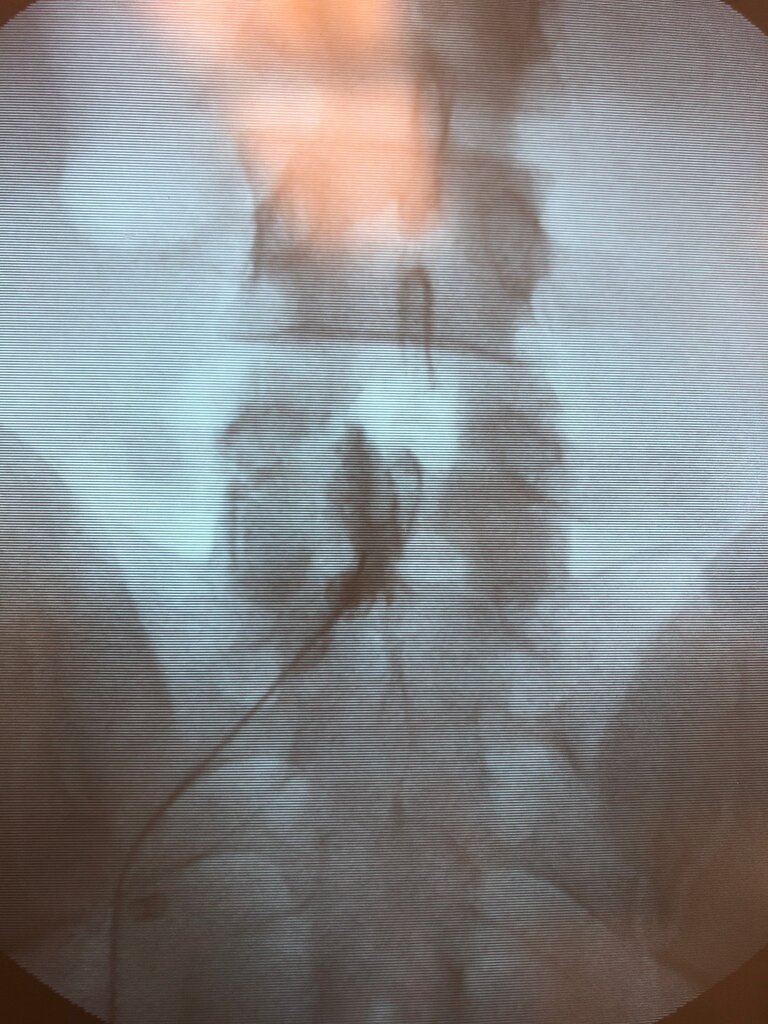
Did an L5-S1 interlam on a seemingly normal 31 year old guy with a central disc at the same level. Calls almost a week later with complaints of severe positional headache not relieved by fluids, caffeine, Tylenol or Advil. Saw him yesterday, says headaches are intermittent but severe and only relieved by ice and laying down. Here are the pics. Doesn’t look like a wet tap at all, but can’t deny the complaints of spinal headache. To blood patch or not to blood patch.
Explained to him in detail my thoughts and how I would advise more time and what he’s been doing. Added fioricet. Any thoughts on this?
Explained to him in detail my thoughts and how I would advise more time and what he’s been doing. Added fioricet. Any thoughts on this?
