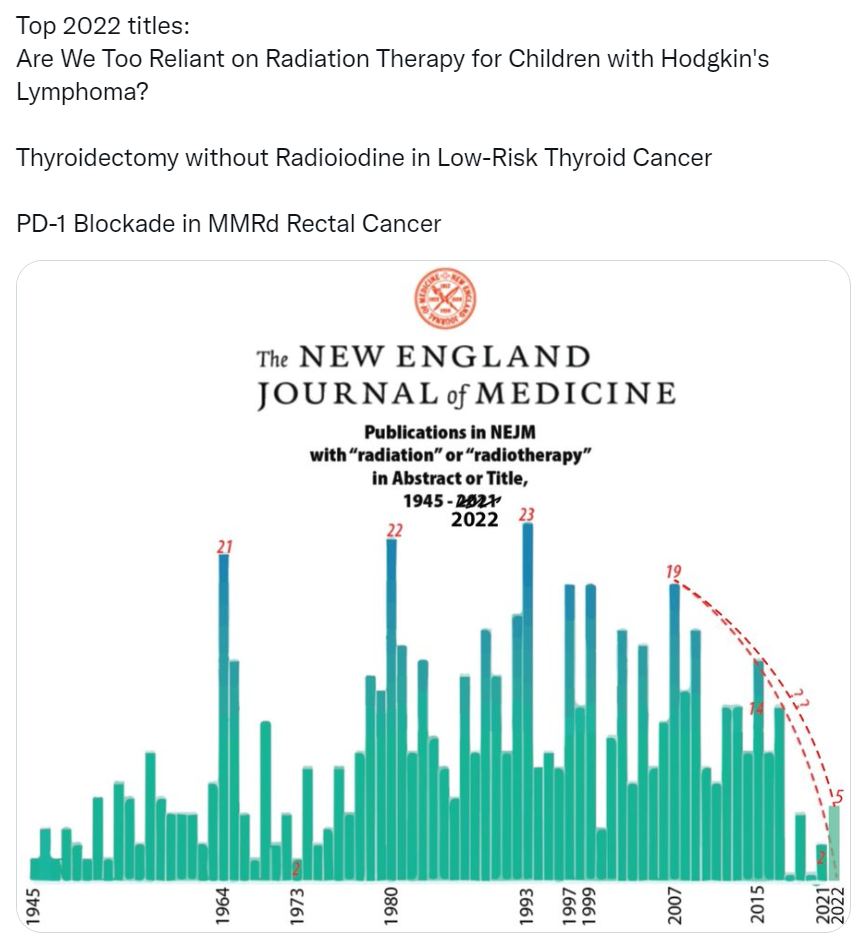
Actually the problem is prioritization and who the burden of proof is on to justify treatment. Why is radiotherapy always targeted for omission?
For breast - other salient questions relative to 'appropriate utilization' could be:
subgroups not requiring endocrine therapy
subgroups not requiring surgery for certain breast atypias
subgroups not requiring breast MRI and extensive and often duplicative imaging such as repeat mammograms, ultrasound, second look imaging, preRT mammogram
plastic surgery and oncoplastic tissue transfer of uncertain oncologic or even cosmetic benefit
rationale for much of neoadjuvant chemotherapy until an overall survival advantage is proven
contralateral mastectomy without survival benefit
I could go on for days. Pretty sure much of this activity is simply accepted as 'standard' local practice. All of these activities generate clinical activity. This logic appears to apply to all specialties except for radiation oncology.