"I know that all oncology fields (medical, surgical, radiation) will all continue to play a large role in cancer treatment and will make advances in their fields," says the OP. However, rad onc's role is diminishing. This is well documented.
And the incidences of our major cancers we treat (prostate, lung e.g.) are declining also. Looked at a certain way...
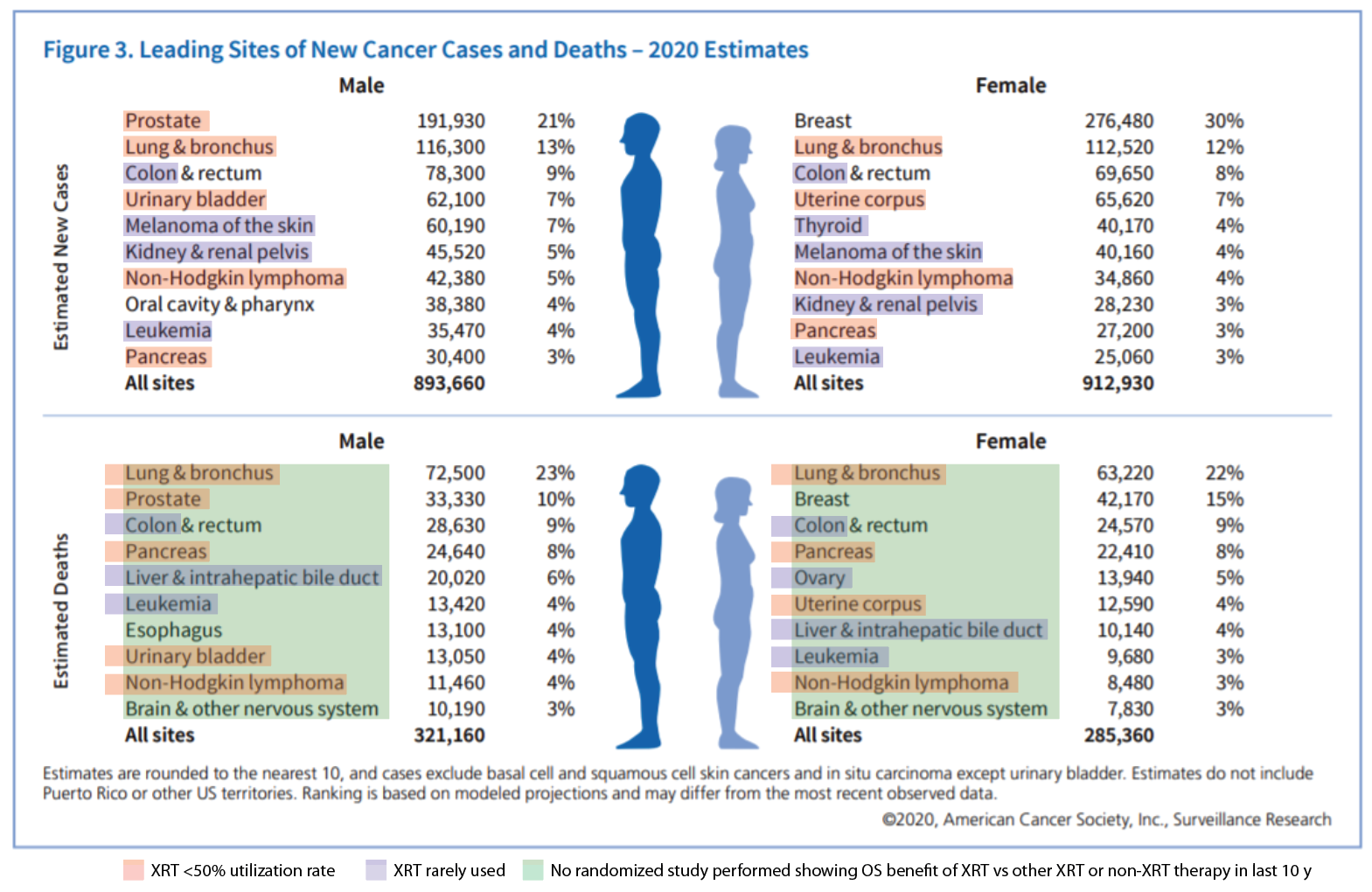
... rad onc doesn't have a very, very large role in "C"ancer therapy (e.g., here's the
RT utilization pattern in stage III uterine over time), and has not been innovating in terms of cancer survival that I can recall. The green shading is a bit of a WAG by me right now but it's not off by much I suppose. (Existentially, of course, given how many rad oncs there are... 1 rad onc for every 6 new pancreas ca patients in the US!... and looking at rad onc utilization... )
There was an interesting review article that came out a couple years ago, "
Practice-changing radiation therapy trials for the treatment of cancer: where are we 150 years after the birth of Marie Curie?"
In it, some of the best minds in the world predicted here's where/how RT would impact cancer therapy in the future:
Improved survival rates are likely to occur through employing/adopting RT in novel situations. There is growing interest in using SBRT to deliver a much higher dose than traditionally given for oligometastatic or oligoprogressive disease; early trials have shown improvements in progression-free survival for this approach. Larger trials aiming to evaluate the role and benefit of ‘radical’ high-dose RT in oligometastatic disease across disease sites are currently underway in the UK (CORE) or in development (ESTRO/EORTC OligoCare studies). SBRT and/or MR-guided RT may also prove beneficial in cancers not traditionally amenable to RT, such as renal and pancreatic cancers, due to the previous inability to irradiate without including large normal tissue margins that precluded the delivery of a tumouricidal dose. Survival may also be improved through dose escalation via improved image guidance (as previously discussed), and novel drug combinations with RT.
IMHO, survival improvements are the "
red rose" of cancer therapy. Will treating mets and rare cancers like pancreas be how rad onc innovates in the next decade?
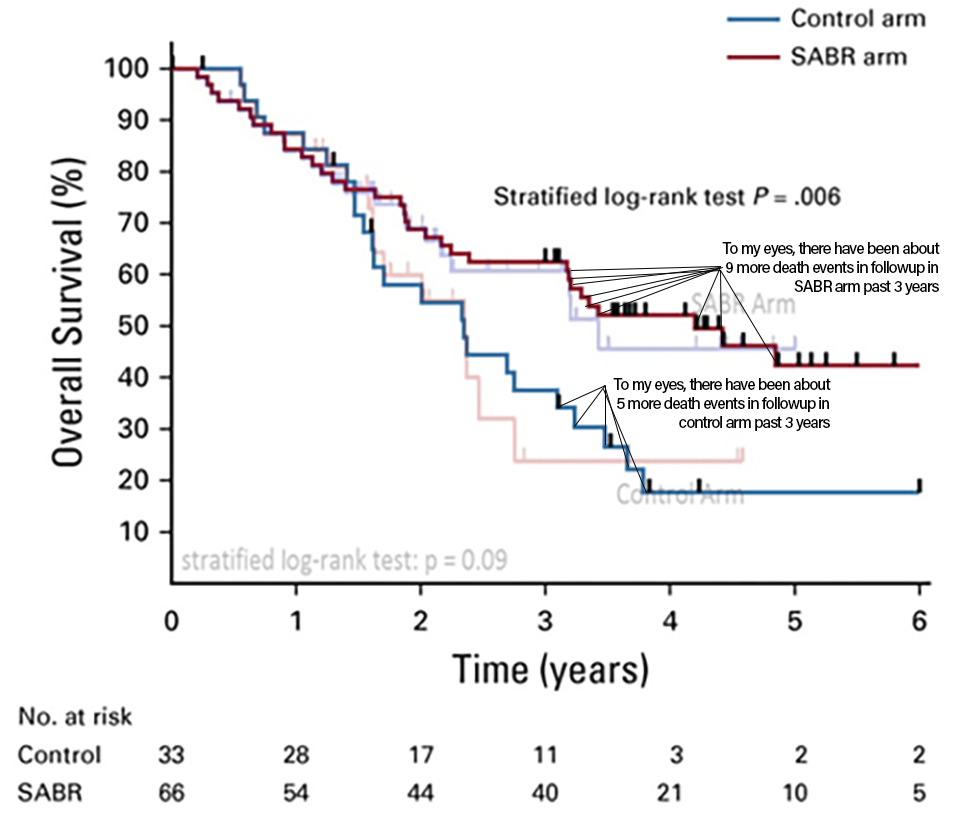
It's tough to improve survival with XRT over and above what we already use it for. We are just not going to see curve separations like
this or
this in XRT, ever. For the last twenty plus years I have been hearing about this unicorny, magical new (non-chemo) drug that will somehow interact with radiation that will make radiation work better. How many hundreds of MD/PhDs have worked on that problem, and how many of these drugs do we use in the clinic daily?
But... keep an eye on FLASH. IF we can offer the same cancer benefit as present-day XRT w/ much less side effects and in a lot fewer fractions, that will be great.
1. Trends in the Utilization of Radiation Therapy (XRT) Among Patients with Non-Hodgkin's Lymphoma (NHL) in the United States (US).
2. What is the optimal radiotherapy utilization rate for lung cancer?—a systematic review.
3. Trends in the use of radiation therapy for stage IIA prostate cancer from 2004 to 2013: a retrospective analysis using the National Cancer Database.
4. Internal mammary and medial supraclavicular lymph node chain irradiation in stage I–III breast cancer (EORTC 22922/10925): 15-year results of a randomised, phase 3 trial.