What a great question.
So let's take MD Anderson's
"Standard Charges" CSV file.
Now, let's do the same math as the
JAMA paper as above:
View attachment 358841
Proposal:
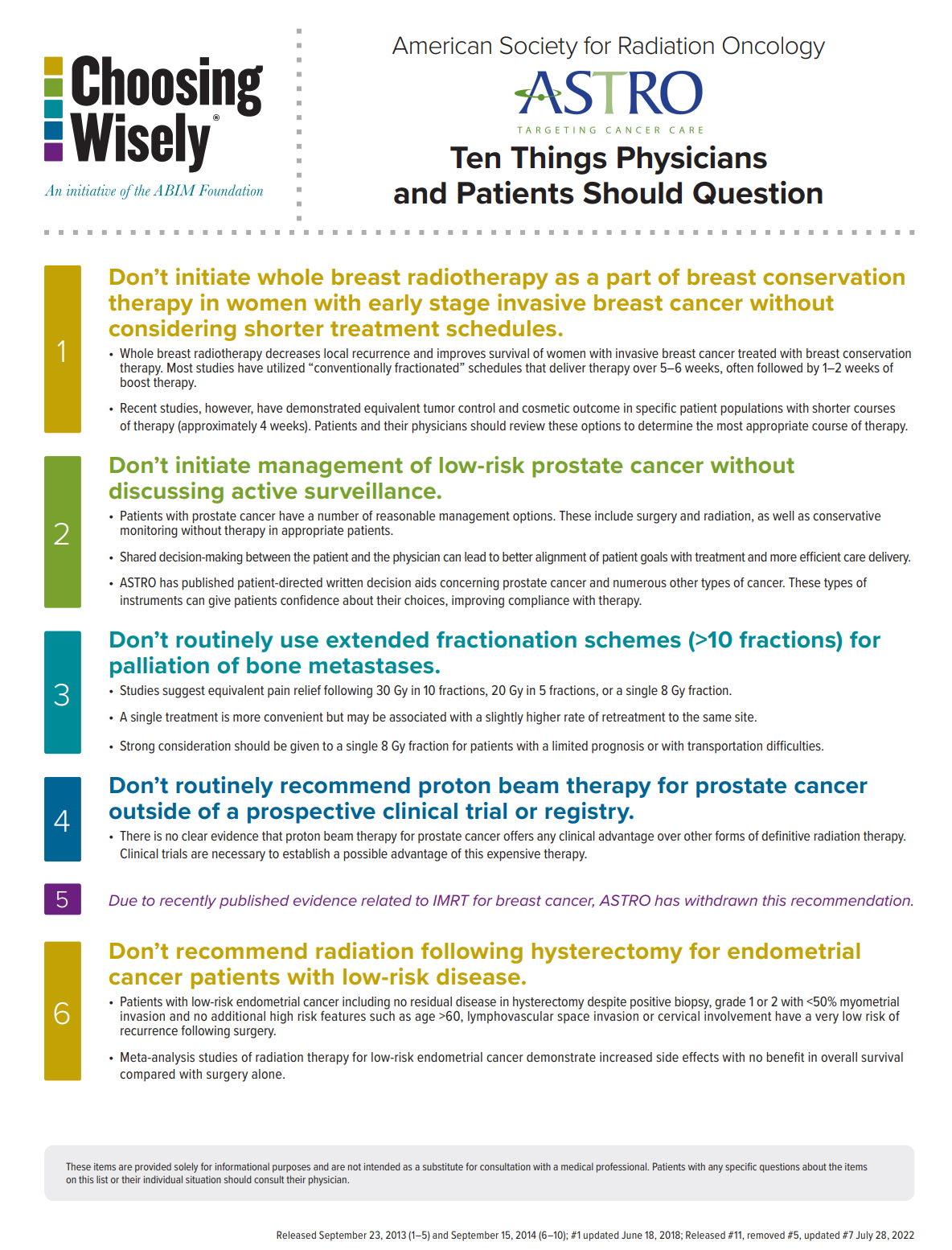
Choosing Wisely #12: Avoid referring patients to PPS-exempt centers whenever possible if you
actually care about financial toxicity.
Charges vs real prices vs financial toxicity to the patient vs global financial toxicity.
These are all different things.
This is how I think entrenched academic docs (who actually think about this stuff, many academic docs appropriately are only concerned about research and patients)/admins and gvt policy makers feel.
1. Except for the VA and NIH affiliated health services, we do not have a national provider, We largely rely on a collection of large, non-profit and sometimes state run, academic medical centers to establish standards of care and drive meaningful medical research.
2. The mission of these centers is nominally to provide tertiary care and establish standards of care through research while providing technical/clinical advances.
Now we know that most of these centers are run with a very corporate model nowadays, where bottom line, expansion and management of endowment become parallel missions.
3. There are fairly nominal differences in CMS compensation across regions/centers with the exception of PPS exempt centers (42% and 37% more from CMS to these centers for inpt and outpt services per 2015 data). CMS justifies this by thinking that they are supporting the greater societal goal of research. It should be noted that most of the most prominent academic research centers are not PPS exempt, and many PPS exempt centers would not qualify as "Top Tier" academic places by most people's standards.
PPS is a boondoggle relic of some congressional funny business/pork from a different era. Even the feds know this, but it is hard to change (congress).
4. The main difference in compensation comes from private payors, where large systems can negotiate crazy rates and the payors themselves may not be incentivized to provide affordable care because of perverse financial incentives and percentage caps on profit. When you negotiate crazy rates, you have to charge close to those rates to collect what you can. I believe this is what drives the differences in these charge masters.
5. The people who write these paternalistic guidelines are overwhelmingly associated with these large academic centers that can negotiate high rates. But, they view these rates as being a
transfer of wealth from insurance companies that are providing products to either wealthy corporate employers or relatively wealthy individuals. That wealthy corporations or individuals may pay more for "premium services" and support the greater societal goal of research is fine by them. It also facilitates the growth of these institutions and their greater control over the field and the provision of "high standard" care.
6. The people who write these guidelines may become fairly wealthy by becoming chairmen or upper admin. There is some pathway to C-suite, and this is some real wealth. But by and large, they can comfort themselves with the idea that they never really worked for money but rather for societal and institutional goals.
7. The people who write these guidelines do know that there are docs out there in the wilderness for whom there is a direct connection between services rendered and income. These docs have a perverse incentive to provide the most expensive care possible, and this needs to be stopped. Historically, many of these wilderness docs were notably more wealthy than their academic peers. This also represented an injustice. To the extent that these guidelines may mitigate any such disparity, all the better.
It would really be a shame if community docs and hospitals did really well treating early stage breast with IMRT.
8. If you are a wilderness (community doc) without a significant professional attachment to collaborative groups or your professional organization, you are a problem in this field. This is not true for larger fields. Most IM docs don't give AF about being a part of collaborative groups, or guideline generation or being seen at a conference. They know that most IM docs need provide care in the community. Academic IM docs are just grateful that they don't have to provide all that care. Because Radonc is such a source of revenue however, academic Radonc has changed this equation. The tacit goal is to provide all radonc care at large academic centers or affiliates.