- Joined
- Jul 16, 2003
- Messages
- 6,030
- Reaction score
- 3,805
70 y/o male scheduled for Adrenalectomy 2/2 pheo.
PMHx:
DCM (EF 25%), CABGx5/MVR, COPD (smoker and barrel chested), PAs 70's/40's, IDDM, Sjogrens, hyperlipidemia.
Pre-op labs: nml except for erythrocytosis with a Hgb of 17.3
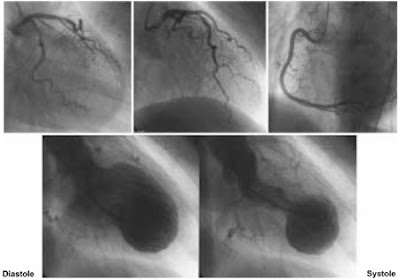
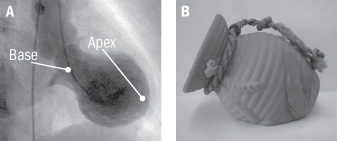
CT:

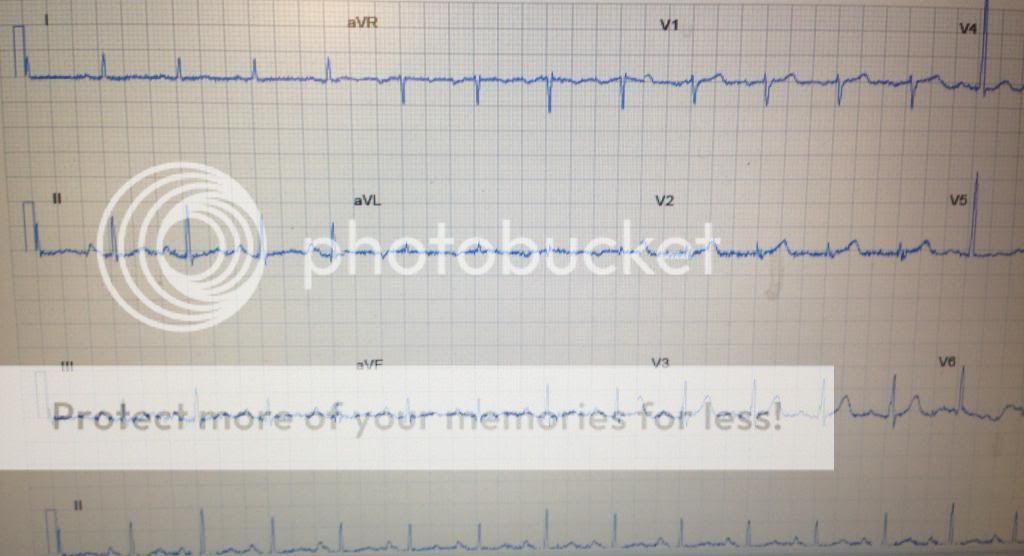
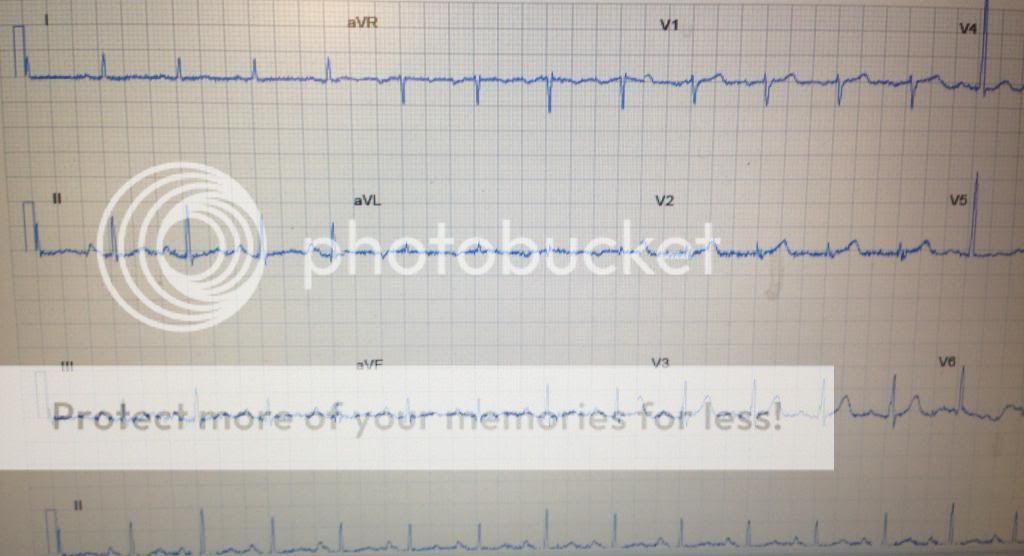
Pre-op EKG:

You induce anesthesia. As the surgeons get to the capsule of the adrenal mass, your rhythm converts to this:
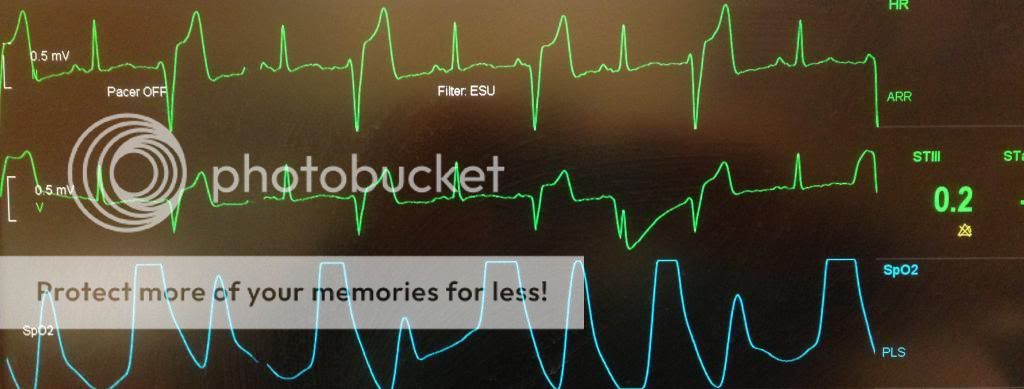
What are your concerns?
PMHx:
DCM (EF 25%), CABGx5/MVR, COPD (smoker and barrel chested), PAs 70's/40's, IDDM, Sjogrens, hyperlipidemia.
Pre-op labs: nml except for erythrocytosis with a Hgb of 17.3
CT:

Pre-op EKG:

You induce anesthesia. As the surgeons get to the capsule of the adrenal mass, your rhythm converts to this:
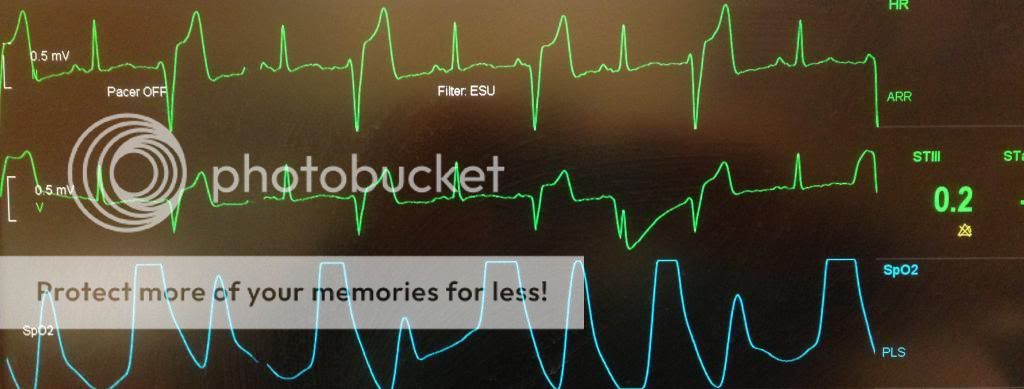
What are your concerns?
Last edited: